Printed from acutecaretesting.org
October 2016
Detection of bacterial infections using PCT and CRP in elderly emergency room patients
Summary Bacterial infections are one of the major reasons for patients presenting to the ED - and the main cause of death in elderly patients. It is important to identify elderly patients with bacterial infections early and initiate treatment in the ED for a better outcome. However, an infection in an elderly patient can be difficult to assess, as symptoms are often atypical.
INTRODUCTION
As a result of the demographic shift the rate of elderly patients presenting to the emergency department is steadily increasing [1]. In western societies elderly patients account for up to a quarter of visits in the emergency department (ED).
The geriatric patient is defined by multimorbidity, functional decline and loss of autonomy [2]. Main presenting causes in the ED are neuropsychiatric disorders, cardiovascular disease, adverse drug effects, abdominal pain, social reasons and infections [3].
Infections are the main causes of death in elderly patients [2]. The mortality risk of patients presenting to the ED increases significantly with age, and it is also affected by the presence of chronic diseases. Coexisting chronic diseases (comorbidities) increase with age and elderly emergency room patients are at higher risk of complications. Major comorbidities that promote an infection in the elderly are diabetes mellitus and the presence of chronic heart failure.
To diagnose and treat infections in elderly emergency patient requires higher effort [4]. They present with "non-specific" and "atypical" symptoms like falls, reduced functionality, shortness of breath, incontinence, syncope, nausea/vomiting or delirium [1]. Infections in the elderly are frequently atypical and non-specific complaints are the reason for presentation, complicating the diagnosis [3].
Geriatric emergency room patients present in up to 20 % of the cases with non-specific symptoms [5]. The median age of patients with non-specific complaints is 82 years and they possess on average four comorbidities. A serious condition is found in 59 % of emergency patients with unspecific complaints [6].
In 14 % a pneumonia and 13 % a urinary-tract infection is the definitive diagnosis [7]. Multiple complex comorbidities further complicate the diagnosis and pre-existing disease have to be distinguished from new acute disease. Elderly emergency patients are frequently undertriaged by triage tools like the „Emergency Severity Index (ESI)“: The high treatment urgency is not recognized [8].
INFECTIONS IN ELDERLY EMERGENCY ROOM PATIENTS
Immunological changes, altered functionality, decreased reserves, multimorbidity and a reduced barrier function of the skin/mucous membranes promote the occurrence of infections in elderly patients [2]. The aging of the immune system is called immunosenescence [9].
Elderly patients with bacterial infections possess a reduced local and systemic response and present with other clinical characteristics than young patients. A classical systemic inflammatory response (body temperature less than 36 °C or greater than 38 °C, heart rate >90 beats per minute, tachypnea >20 breaths per minute, white blood cell count less than 4,000 cells/mm³ or greater than 12,000 cells/mm³) is often not observed.
The most common infections in elderly patients are urinary-tract infections (22 %), pneumonia (25 %) and sepsis/bacteremia (18 %) [3].
In emergency medicine it is an essential aim to quickly diagnose time-critical diseases, carry out risk stratification and treat the disease. To diagnose infections in elderly emergency room patients is difficult for health professionals [1]. Signs and symptoms of infections in elderly emergency patients are more subtle and masked compared to younger patients and therefore the affected vulnerable patients need to be examined more carefully.
In patients with non-specific complaints the correct diagnosis pneumonia was found in 68 % and a urinary-tract infection in 47 % in the emergency department when compared with the hospital discharge diagnose, demonstrating the diagnostic difficulties [10].
Elderly emergency room patients with community-acquired pneumonia (CAP), for example, do not present with classical symptoms such as fever, cough and/or sputum. Rather, they present with acute respiratory distress and impaired consciousness or with other types of symptom (reduced functionality or impaired chronic diseases) [11].
Pathological changes in vital parameters are often less pronounced or can be completely missing in the elderly [12]. For example, tachycardia can be absent in serious infections and sepsis [3]. A key criterion for the diagnosis of an acute infection is the increased core body temperature. The cardinal symptom of a bacterial infection fever is absent in about 30 % of all cases [13].
Elderly patients with pneumonia present in a significant percentage (up to 36 %) without an elevated body temperature [11, 14]. This can be partially explained by the limit of fever (limits inconsistently defined with 38 °C or 38.3 °C) not being specific for the elderly [15].
In a prospective study in unselected emergency patients older than 75 years, it was demonstrated that a tympanal measured body temperature higher than 37.3 °C and a rectally measured body temperature higher than 37.8 °C can already be interpreted as a sign of a bacterial infection [16].
A qualitative disturbance of consciousness, such as acute confusion or altered vigilance as part of delirium is one of the most important manifestations of atypical complaints in the elderly, which is often associated with an infection [17]. In the absence of fever, the presence of a delirium is often the only symptom of acute infection among the elderly.
PCT AND CRP AS BIOMARKERS OF BACTERIAL INFECTIONS IN ELDERLY EMERGENCY ROOM PATIENTS
Elderly emergency patients presenting with atypical symptoms need to be examined carefully. There is an essential relevance for the use of biomarkers of bacterial infections in ED: A recent study has shown that current cut-off levels of body temperature are not reliable parameters for diagnosing bacterial infections in elderly patients [16]. Also the leukocyte count is an unreliable parameter in elderly patients. Leukocytosis may initially be absent or only minimally changed [11].
In elderly patients with cholecystitis no leukocytosis increase was found in 41 % [18]. In elderly patients with pneumonia a seven-fold increased mortality was found in patients without leukocytosis. A reduced or absent systemic inflammatory response is therefore an important factor that is associated with an increased mortality [19].
It is therefore essential to identify elderly patients without systemic inflammatory response at an early stage in order to reduce the risk of death.
An opportunity for the detection of an infection is the use of biomarkers. Six hours after a bacterial infection CRP begins to rise and the peak is reached after 48 hours [9]. CRP possesses a half-life of 19 hours.
The half-life of CRP is not influenced by comorbidities and can hence be used for therapeutic monitoring in the elderly. In elderly patients there is a reduced CRP response to bacterial infections, but without clinical significance [20]. In elderly emergency patients CRP is a useful biomarker to predict early bacterial infection with higher sensitivity compared to leukocyte count [21].
In addition, the use of procalcitonin (PCT) is a valuable diagnostic alternative in the evaluation of acute infections, reflecting the prognosis and severity of pneumonia even in elderly patients [22]. In a recent meta-analysis diagnostic accuracy of PCT was not inferior in elderly patients with sepsis compared to younger patients; hence it is not influenced by immunosenescence [23].
The overall sensitivity and specificity was 83 %. Of note, CRP levels displayed a higher sensitivity (91 %), but a lower specificity (36 %) compared to PCT. Subsequently, the authors conclude that PCT is helpful for the diagnosis of sepsis in elderly patients.
Due to the imperfect diagnostic accuracy, PCT levels in the elderly should always be interpreted in the context of clinical findings. Specifically, the use of biomarkers in elderly patients in the emergency room may help to recognize a severe infection, adds information to the clinical finding and helps initiate the necessary treatment.
In elderly emergency room patients with non-specific symptoms (described above) a bacterial infection should always be considered in the differential diagnosis and biomarkers could be used to facilitate the diagnosis. In the ED it has been demonstrated that implementation of standardized care bundles for the predominant ED infection community-acquired pneumonia is associated with a 21 % relative risk reduction of in-hospital mortality [24].
Standardization of diagnostic and therapeutic processes in the ED improves outcome of patients hospitalized for CAP. Indeed, the determination of an inflammation parameter (CRP or PCT) in serum at admission and during the course of 3-5 days is recommended in the German S3 guideline of the competence network CAPNETZ for pneumonia [25].
Recognizing infections in elderly emergency patients is a complex task that needs to take into account non-specific symptoms, vital signs, laboratory values including biomarkers (CRP and PCT), the pre-existing functionality of the patients, worsening of comorbidities and acute changes of the mental status [1]. In the presence of an infection this multimodal approach allows doctors to begin empirically calculated anti-infective therapy as early as possible, see Fig. 1 for an overview.
FIG. 1: Detection of bacterial infections in elderly emergency room patients. Different variables should be considered in diagnostic decision making within the clinical context.
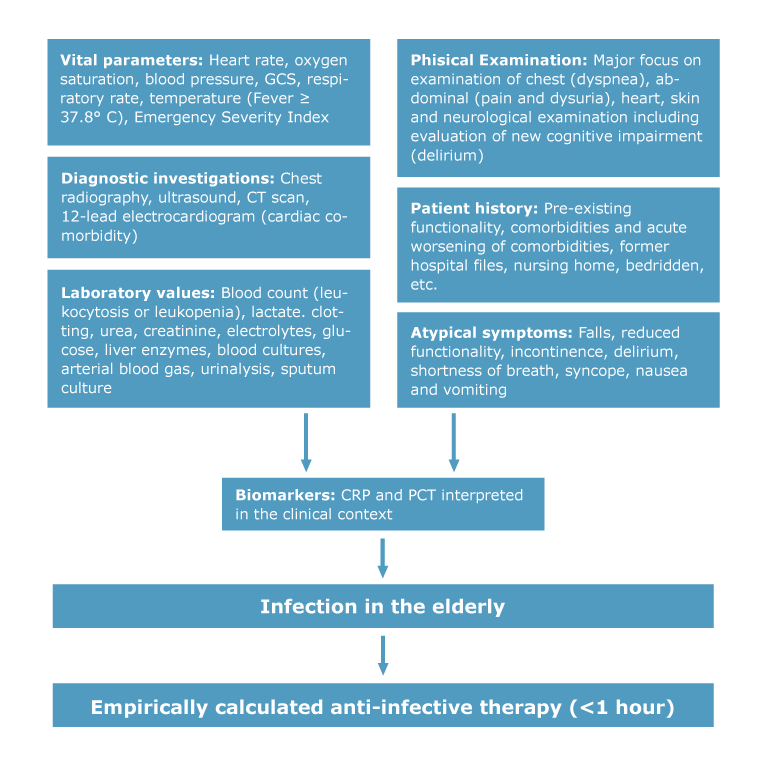
CT ~ computerized tomography
GCS ~ Glasgow coma score
CONCLUSION
Due to demographic change emergency departments face an increasing need for care of elderly patients. Acute infections are the main cause of death in the elderly. The recognition of the vital threat and the diagnosis of infections in elderly emergency patients is a complex task and even subtle changes in the clinical status must be considered.
For the diagnosis of an infection, non-specific symptoms, vital signs, laboratory values, the pre-existing functionality, worsening of comorbidities and acute mental status changes must be taken into account [1]. If an infection is assumed in an elderly emergency room patient, PCT or CRP must be measured and interpreted in the clinical context.
In the presence of an infection it is essential to initiate the empirically calculated anti-infective therapy promptly in a standardized manner. Geriatric emergency expertise is of major importance to solve this difficult task.
References+ View more
- Hortmann M, Singler K, Geier F, Christ M. [Recognition of infections in elderly emergency patients]. Z Gerontol Geriatr 2015; 48: 601-07.
- Heppner HJ, Cornel S, Peter W, Philipp B, Katrin S. Infections in the elderly. Crit Care Clin 2013; 29: 757-74.
- Samaras N, Chevalley T, Samaras D, Gold G. Older patients in the emergency department: a review. Ann Emerg Med 2010; 56: 261-69.
- Singler K, Christ M, Sieber C, Gosch M, Heppner HJ. [Geriatric patients in emergency and intensive care medicine]. Internist (Berl) 2011; 52: 934-38.
- Ruedinger JM, Nickel CH, Maile S, Bodmer M, Kressig RW, Bingisser R. Diuretic use, RAAS blockade and morbidity in elderly patients presenting to the Emergency Department with non-specific complaints. Swiss Med Wkly 2012; 142: w13568.
- Nemec M, Koller MT, Nickel CH, Maile S, Winterhalder C, Karrer C, Laifer G, Bingisser R. Patients presenting to the emergency department with non-specific complaints: the Basel Non-specific Complaints (BANC) study. Acad Emerg Med 2010; 17: 284-92.
- Bhalla MC, Wilber ST, Stiffler KA, Ondrejka JE, Gerson LW. Weakness and fatigue in older ED patients in the United States. Am J Emerg Med 2014; 32(11): 1395-98.
- Grossmann FF, Zumbrunn T, Ciprian S, Stephan FP, Woy N, Bingisser R, Nickel CH. Undertriage in older emergency department patients – tilting against windmills? PLoS One 2014; 9: e106203.
- Bertsch T, Triebel J, Bollheimer C, Christ M, Sieber C, Fassbender K, Heppner HJ. C-reactive protein and the acute phase reaction in geriatric patients. Z Gerontol Geriatr 2015; 48: 595-600.
- Peng A, Rohacek M, Ackermann S, Ilsemann-Karakoumis J, Ghanim L, Messmer AS, Misch F, Nickel CH, Bingisser R. The proportion of correct diagnoses is low in emergency patients with nonspecific complaints presenting to the emergency department. Swiss Med Wkly 2015; 145: w14121.
- Simonetti AF, Viasus D, Garcia-Vidal C, Carratala J. Management of community-acquired pneumonia in older adults. Ther Adv Infect Dis 2014; 2: 3-16.
- Hogan TM, Losman ED, Carpenter CR, Sauvigne K, Irmiter C, Emanuel L, Leipzig RM. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med 2010; 17: 316-24.
- Norman DC. Fever in the elderly. Clin Infect Dis 2000; 31: 148-51.
- Riquelme R, Torres A, el-Ebiary M, Mensa J, Estruch R, Ruiz M, Angrill J, Soler N. Community-acquired pneumonia in the elderly. Clinical and nutritional aspects. Am J Respir Crit Care Med 1997; 156: 1908-14.
- Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 2013; 39: 165-228.
- Singler K, Bertsch T, Heppner HJ, Kob R, Hammer K, Biber R, Sieber CC, Christ M. Diagnostic accuracy of three different methods of temperature measurement in acutely ill geriatric patients. Age Ageing 2013; 42: 740-46.
- Christ M, Popp S, Erbguth E. Algorithmen zur Abklärung von Bewusstseinsstörungen in der Notaufnahme. Intensivmedizin und Notfallmedizin 2010; 47: 83-93.
- Parker LJ, Vukov LF, Wollan PC. Emergency department evaluation of geriatric patients with acute cholecystitis. Acad Emerg Med 1997; 4: 51-55.
- Ahkee S, Srinath L, Ramirez J. Community-acquired pneumonia in the elderly: association of mortality with lack of fever and leukocytosis. South Med J 1997; 90,3: 296-98.
- Wester AL, Blaasaas KG, Wyller TB. Is the concentration of C-reactive protein in bacteraemia associated with age? Immun Ageing 2008; 5: 8.
- Liu A, Bui T, Van Nguyen H, Ong B, Shen Q, Kamalasena D. Serum C-reactive protein as a biomarker for early detection of bacterial infection in the older patient. Age Ageing 2010; 39: 559-65.
- Heppner HJ, Bertsch T, Alber B, Esslinger AS, Dragonas C, Bauer JM, Sieber CC. Procalcitonin: inflammatory biomarker for assessing the severity of community-acquired pneumonia--a clinical observation in geriatric patients. Gerontology 2010; 56: 385-89.
- Lee SH, Chan RC, Wu JY, Chen HW, Chang SS, Lee, CC. Diagnostic value of procalcitonin for bacterial infection in elderly patients - a systemic review and meta-analysis. Int J Clin Pract 2013; 67: 1350-57.
- Hortmann M, Heppner HJ, Popp S, Lad T, Christ M. Reduction of mortality in community-acquired pneumonia after implementing standardized care bundles in the emergency department. Eur J Emerg Med 2014; 21: 429-35.
- Hoffken G, Lorenz J, Kern W, Welte T, Bauer T, Dalhoff K, Dietrich E, Ewig S, Gastmeier P, Grabein B, Halle E, Kolditz M, Marre R, Sitter H. Guidelines of the Paul-Ehrlich-Society of Chemotherapy, the German Respiratory Diseases Society, the German Infectious Diseases Society and of the Competence Network CAPNETZ for the Management of Lower Respiratory Tract Infections and Community-acquired Pneumonia. Pneumologie 2010; 64: 149-54.
References
- Hortmann M, Singler K, Geier F, Christ M. [Recognition of infections in elderly emergency patients]. Z Gerontol Geriatr 2015; 48: 601-07.
- Heppner HJ, Cornel S, Peter W, Philipp B, Katrin S. Infections in the elderly. Crit Care Clin 2013; 29: 757-74.
- Samaras N, Chevalley T, Samaras D, Gold G. Older patients in the emergency department: a review. Ann Emerg Med 2010; 56: 261-69.
- Singler K, Christ M, Sieber C, Gosch M, Heppner HJ. [Geriatric patients in emergency and intensive care medicine]. Internist (Berl) 2011; 52: 934-38.
- Ruedinger JM, Nickel CH, Maile S, Bodmer M, Kressig RW, Bingisser R. Diuretic use, RAAS blockade and morbidity in elderly patients presenting to the Emergency Department with non-specific complaints. Swiss Med Wkly 2012; 142: w13568.
- Nemec M, Koller MT, Nickel CH, Maile S, Winterhalder C, Karrer C, Laifer G, Bingisser R. Patients presenting to the emergency department with non-specific complaints: the Basel Non-specific Complaints (BANC) study. Acad Emerg Med 2010; 17: 284-92.
- Bhalla MC, Wilber ST, Stiffler KA, Ondrejka JE, Gerson LW. Weakness and fatigue in older ED patients in the United States. Am J Emerg Med 2014; 32(11): 1395-98.
- Grossmann FF, Zumbrunn T, Ciprian S, Stephan FP, Woy N, Bingisser R, Nickel CH. Undertriage in older emergency department patients – tilting against windmills? PLoS One 2014; 9: e106203.
- Bertsch T, Triebel J, Bollheimer C, Christ M, Sieber C, Fassbender K, Heppner HJ. C-reactive protein and the acute phase reaction in geriatric patients. Z Gerontol Geriatr 2015; 48: 595-600.
- Peng A, Rohacek M, Ackermann S, Ilsemann-Karakoumis J, Ghanim L, Messmer AS, Misch F, Nickel CH, Bingisser R. The proportion of correct diagnoses is low in emergency patients with nonspecific complaints presenting to the emergency department. Swiss Med Wkly 2015; 145: w14121.
- Simonetti AF, Viasus D, Garcia-Vidal C, Carratala J. Management of community-acquired pneumonia in older adults. Ther Adv Infect Dis 2014; 2: 3-16.
- Hogan TM, Losman ED, Carpenter CR, Sauvigne K, Irmiter C, Emanuel L, Leipzig RM. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med 2010; 17: 316-24.
- Norman DC. Fever in the elderly. Clin Infect Dis 2000; 31: 148-51.
- Riquelme R, Torres A, el-Ebiary M, Mensa J, Estruch R, Ruiz M, Angrill J, Soler N. Community-acquired pneumonia in the elderly. Clinical and nutritional aspects. Am J Respir Crit Care Med 1997; 156: 1908-14.
- Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 2013; 39: 165-228.
- Singler K, Bertsch T, Heppner HJ, Kob R, Hammer K, Biber R, Sieber CC, Christ M. Diagnostic accuracy of three different methods of temperature measurement in acutely ill geriatric patients. Age Ageing 2013; 42: 740-46.
- Christ M, Popp S, Erbguth E. Algorithmen zur Abklärung von Bewusstseinsstörungen in der Notaufnahme. Intensivmedizin und Notfallmedizin 2010; 47: 83-93.
- Parker LJ, Vukov LF, Wollan PC. Emergency department evaluation of geriatric patients with acute cholecystitis. Acad Emerg Med 1997; 4: 51-55.
- Ahkee S, Srinath L, Ramirez J. Community-acquired pneumonia in the elderly: association of mortality with lack of fever and leukocytosis. South Med J 1997; 90,3: 296-98.
- Wester AL, Blaasaas KG, Wyller TB. Is the concentration of C-reactive protein in bacteraemia associated with age? Immun Ageing 2008; 5: 8.
- Liu A, Bui T, Van Nguyen H, Ong B, Shen Q, Kamalasena D. Serum C-reactive protein as a biomarker for early detection of bacterial infection in the older patient. Age Ageing 2010; 39: 559-65.
- Heppner HJ, Bertsch T, Alber B, Esslinger AS, Dragonas C, Bauer JM, Sieber CC. Procalcitonin: inflammatory biomarker for assessing the severity of community-acquired pneumonia--a clinical observation in geriatric patients. Gerontology 2010; 56: 385-89.
- Lee SH, Chan RC, Wu JY, Chen HW, Chang SS, Lee, CC. Diagnostic value of procalcitonin for bacterial infection in elderly patients - a systemic review and meta-analysis. Int J Clin Pract 2013; 67: 1350-57.
- Hortmann M, Heppner HJ, Popp S, Lad T, Christ M. Reduction of mortality in community-acquired pneumonia after implementing standardized care bundles in the emergency department. Eur J Emerg Med 2014; 21: 429-35.
- Hoffken G, Lorenz J, Kern W, Welte T, Bauer T, Dalhoff K, Dietrich E, Ewig S, Gastmeier P, Grabein B, Halle E, Kolditz M, Marre R, Sitter H. Guidelines of the Paul-Ehrlich-Society of Chemotherapy, the German Respiratory Diseases Society, the German Infectious Diseases Society and of the Competence Network CAPNETZ for the Management of Lower Respiratory Tract Infections and Community-acquired Pneumonia. Pneumologie 2010; 64: 149-54.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info.
Acute care testing handbook
Get the acute care testing handbook
Your practical guide to critical parameters in acute care testing.
Download nowScientific webinars
Check out the list of webinars
Radiometer and acutecaretesting.org present free educational webinars on topics surrounding acute care testing presented by international experts.
Go to webinars










