Printed from acutecaretesting.org
July 2010
Lean as a learning system in a hospital ward
Lean in healthcare
Lean is rapidly becoming the latest rage in healthcare as it diffuses out of the automotive industry towards other environments (Jones and Mitchell, 2006). As a result, hospital staff are now experiencing the same frustrating difficulties with lean that have previously plagued lean transformations in industry.
Namely, lean advocates are so focused on “process improvement” they sometimes lose their perspective on the fact that for any process to perform better the people who compose the process need to be better at what they do. In that sense, lean is a learning method more than anything else.
As we have argued elsewhere, the first practitioners of lean in Toyota, all these years ago, conceived of lean as a way to “develop kaizen mentality in every employee,” rather than “applying lean tools to every process” (Ballé et al., 2006).
Three years ago, one of the authors, the head of nursing at the hospital Nord 92 in Villeneuve-La-Garenne, in the northern outskirts of Paris approached the founders of the Projet Lean Entreprise, France’s leading academic lean initiative at Te´le´com Paris to apply to the wards a “lean” approach, in the spirit of the work previously done in several French hospitals (Ballé and Champion-Daviller, 2004).
Indeed, “lean thinking”, derived from the famed Toyota Production System is well adapted to solve the operational problems presented by organizing the work of a large number of staff with a great variety of patients in a very demanding environment. It’s double focus on customer satisfaction and employee involvement also suits the work culture of most care centers.
However, experience shows that the interpretation of lean concepts and tools outside of the automotive industry is a critical challenge and its success largely rests on understanding first that lean is a system, not simply a toolbox, and second that this system must be constructed by the ward managers, matrons and nurses themselves rather than the piecemeal application of industrial practices to the wards.
Indeed lean is a learning system from which the patients’ benefits through greater safety and shorter lead times, as well as the nursing profession itself, through a better understanding and mastery of its own practices.
Lean is a system of thinking, not a set of tools
As many lean experts remind us, lean is a system, and applied piecemeal, although the tools deliver local results almost without fail, these improvements are rarely sustained. Over relatively short periods of time (six months to one year) early enthusiasm is likely to yield to frustration and then to cynicism, until people start looking for the next best thing.
The various lean “tools” and “principles” are tightly interconnected. For instance, to illustrate this in a hospital context, let’s think about the “simplest” of the lean tools: 5S (sort and eliminate, straighten, shine, standardize and sustain), which is traditionally considered a good starting point for kaizen activities.
In most wards, the immediate reaction of improvement teams to 5S exercises is to complain of the structural lack of storage space, and usually rightly so, many wards having been designed without much consideration for material and supply storage.
Although some progress can be achieved with basic 5S, the fact remains that in many cases the inventory, which the ward needs to hold, simply overflows in the available space. Which is why just-in-time is required. In many cases, the stock of supplies corresponds to a weekly delivery, which obviously floods the ward with products.
Progress on the just-in-time principle of, for instance, daily deliveries solves the space problem immediately. However, daily deliveries would mean far less stock on hand, so a much greater reactivity from the nursing teams to any risk of supply failure. This, in turn, demands a rigorous application of the “jidoka”, or “react at first defect” second pillar of the lean system, to make sure corrective action is triggered at the very first risk of missing products.
In this illustration, it is clear that working endlessly at 5S without tackling the just-in-time element will soon become frustrating because of material constraints (size of inventory vs size of cupboards), but reducing the inventory and increasing the delivery can augment patient risk if it is not strongly accompanied with an increase of reactivity both from the nursing and delivery staff (Figure 1).
In this sense, lean is a learning system which encourages staff to perform better in technical operations, which, in turn, increases process performance.
FIG. 1: The lean system
However, as Art Smalley has repeatedly shown, this learning cannot occur if basic stability has not been achieved (www.superfactory.com/articles/Smalley_Basic_ Stability.htm). Any complex system, such as ward organization, is likely to suffer from the pillowcase syndrome: squeeze one end, and it bulges at another.
In other words, in a chaotic environment, any “improvement” activity can easily shift the burden to another element of the system, which will then collapse, often cancelling the initial positive results. In lean, basic stability is absolutely essential to create the proper learning environment where employees can see clearly the impact of their actions and then learn through the kaizen activities, not simply make the problems go away.
The need for basic stability is well understood in healthcare applications of lean, and indeed, Steven Spear has argued that successful lean implementations in healthcare are essentially about reducing ambiguity in the wards. For this author, the aim of the Toyota production system is to turn workers into problem-solvers, and doing so in complex environments such as hospitals is about educating people to stop going around problems, but fixing them now!
To do so, their working environment must enable them to see clearly what is a problem and what is not, or, in the words of a Toyota expert, to identify abnormal conditions at a glance. In practice, this turns out to be a lot harder in a hospital ward that one might think.
Firstly, a lot of people are doing many independent tasks at any one time. Are the laundry bags piled up in front of the elevator normal conditions because they are just being taken down, or have they been lying there since early this morning? Is the wheelchair parked against the wall at its normal place, or has it just been left there? Is a patient complaining loudly about a nurse a reflection of this person’s pain, bad manners, or a legitimate complaint about the way he or she has been treated by the hospital staff?
Considering the high number of activities to coordinate at a given time, the equally high number of staff, both full-time and agency, and the inherent challenges of dealing with patients’ health and suffering, many of the simplest tasks can become inordinately complicated, and it can seem dauting to maintain “normal conditions.”
Nonetheless, this is the approach Nord 92 has chosen to take to implement lean. Led by one of the authors, the nursing staff had identified a number of complex nursing issues, such as medication distribution errors, catheter infections, nosocomial infections, bedsores: the usual assortment of headaches one will find in many wards.
However, having tried to tackle these problems head-on for many years, they determined to attack the issue differently and start by focusing on basic stability. In the past, their improvement efforts had been frustrated by the annoying real-life fact that every incident analysis had unveiled a different cause.
In trying to solve causes one after the other, they had increased the overall weigh of procedures and work instructions without really solving any of the recurrent problems.
Basic stability
Furthermore, the head nurse and the nursing managers also reasoned that by first applying “basic stability” to their working environment, they could then move on to improving more technical work involving direct patient contact. Consequently, they started with an apparently banal task: maintaining empty corridors.
From a safety point-of-view, this makes obvious sense since any object, such as beds, trays, chariots, wheelchairs etc., can easily roll and block emergency exit in a panic in case of a fire or any other need to evacuate. Keeping the corridors clear seemed also to be a pretty simple task without any technical difficulties. Not so.
It quickly appeared that the reason things were kept in the corridors was because there was no storage space available elsewhere. The nursing management team had to come to terms with the fact that solving this simple problems would lead to attack seriously the question of 5S in the storage areas.
In some specific instances this led to problem solving with the nursing teams themselves when rest areas had to be reconfigured to accomodate rolling beds and other appliances. By example, one old bookshelf was entirely dismantled in order to make room for several wheelchairs and so on.
On the plus side, the nursing teams having participated to the problem-solving exercise, maintaining the corridors clear became less of a discpline issue than previously (Plate 1). Nonetheless, some specific issues, such as where to put the dirty laundry bins remain unresolved three years down the line, and a group is working on looking at the entire flow of clean vs dirty material.
Focusing on the “clear corridor” problem, the nursing managers came to realize that they kept bumping into nursing trolleys full of material, which staff assured them had been cleaned at the end of the shift. Further investigation led to the practical conclusion that the only “guarantee” a trolley had been effectively cleaned was that it had been completely emptied of all its content after use.
Again, this apparently simple policy unearthed a further issue, which was the general question of material handling. People kept what they needed on the trolleys, because in that way, they felt certain they would have everything at hand, and no longer need to look for stuff all the time. This apparently mundane problem convinced the management team they needed to tackle seriously the storage issue.
They started with a systematic audit of what was kept where and discovered, unsurprisingly, too much of some things, not enough of others, multiple holding points, hidden reserves, dangerous locations (top of shelves, corners, etc.).
Far more worrisome, their search for working material unearthed a number of out-of-date products lurking in the stock accumulations. Increasingly worried, they then focused on this issue with material supplies, and slowly grasped the extent of the quality problem.
In essence, they were relying on the thoroughness of the nursing personnel to check whether products where not out-of-date at the point of use. In other words, they were laying traps for their own staff, and their patients!

PLATE 1: Maintaining the corridors
This initial audit led to a “zero out-of-date” challenge for all the wards, as well as a “supermarket” policy in storage areas. Each point of storage had to resemble a supermarket, with rows of products clearly identified, and the newest deliveries placed at the back of the queue.
To achieve this, each nursing team had to work at understanding daily consumption of each product, and set stock levels accordingly. Even this was not easy. After an initial success, the storage policy faltered six months later until the nursing managers accepted the need to recalculate all the stock levels on a quarterly basis to allow for the constant change in patient population, and hence the varying level of needs for various products.
In lean terms, the nursing managers and their teams learn to experiment with leveling. A clear benefit of the “supermarket” approach is that anything out of place stands out, and in particular suspicious products (old packaging, open bottles, etc.), which makes it easier to systematically look out for aging products and out-of-dates (Plate 2).
In the end, the nursing managers adopted the practice of a daily tour of the wards following a basic checklists of spot checks to make sure the ward was maintained in “normal conditions.” Furthermore, they worked with the nursing staff so that any problem be tackled immediately, trying to get back to standard.
In doing so a variety of concerns emerged which had not been seen as such beforehand, such as the systematic cleaning of the material used by the physiotherapists, or a more rigorous handling of food circuits in the wards. The other side-effect was that old or damaged material became more apparent.
Cardboard boxes, for instance, a known source of germ retention, were progressively replaced by plastic containers. Broken armchairs were replaced, damaged fixtures repaired and so forth. In the end, emptied, cleaned nursing trolleys eventually found their place in cleared out cupboards, so as to avoid encumbering the wards’ corridors (Plate 3).

PLATE 2: The "supermarket" approach

PLATE 3: Nursing trolley in a cleared out cupboard
Standardizing nursing practices
After focusing for about a year on maintaining their working environment, the nursing management team then made a fundamental leap forward. If the “regular tour with checklist” approach had worked on ward environment, surely the same thing could be applied to nursing itself.
Having clarified the wards and sustained a basic discipline in their working areas, the nursing managers were ready to tackle basic stability in the nursing care itself. Traditionally, in France, this is considered a delicate area because nurses tend to be very defensive of their skills, and consider that once they have graduated from nursing school their experience is the only source of progress.
Although nurses follow many programs of classroom training, there is no tradition of “on the job” training, and the whole issue of skill levels tends to be taboo.
In this instance, nursing staff had grown accustomed to the use of checklists on the environment. They were generally skeptical about using the same approach to themselves, but they agreed to work with the nursing managers to establish at least one checklist on basic patient care, to see what could be included in this list.
In practice, the first checklist was much easier to build than anticipated since all the nurses shared a pretty good idea of what they were supposed to do. Having constructed the list with the ward managers, they agreed to experiment with systematic observation of actual care in practice. Each ward manager undertook to observe 20 practices according to the checklist.
The upshot of this experiment was that although the nurses knew what they had to do, in real life nursing, they tended to skip many of the steps for a variety of reasons. They would not look at the individualized care plan because they felt they knew the patient already. They failed to wash their hands because it simply slipped their minds.
In other cases, they skipped some items because of specific difficulties, and the need to keep the rhythm of the care moving. All in all, most nurses felt the exercise was an eye-opener and became quite curious about the overall results.
In their respective wards (the checklists varied slightly from one ward to the other because of different care specialties), the managers then established a Pareto of issues in basic care, and discussed with their teams what could be done about the top three items.
After a few months of working with their teams on the problems, the nursing managers ran a second observation, and problems identified were reduced in some instances by as much as 80 percent.
At this later stage, on basic care at least, the wards developed actual nursing standards using the TPS format for work standards, and they now use this document to check how agency staff works with patients (Figure 2).
Having successfully tackled basic care, the teams started the same process for more technical care, such as bandages, catheter insertion and so on. When the lean initiative got off the ground, the hospital’s nursing manager started monitoring main incidents monthly with the ward managers, in terms of nosocomial infections, catheter infections, medication errors, medication reactions, falls, complaints, etc.
Over the first two years, the rate of incidents per patient halved (that is, the probability each patient admitted has of facing an incident reduced by 45 percent). These outstanding results also helped answer another vexing question. At the start of the work, the head nurse wondered whether she should start with the entire hospital upfront, or begin with a local pilot.
The lean lesson learned here is that, indeed, better imperfect lean techniques applied systematically rather than perfect ones applied sporadically. Much of the success in the wards is due to the systemic improvements obtained by getting the entire hospital to progress at the same time (in fact, administrative and pharmacy managers were also part of the implementation team).
Moving on to complex problem solving
Certainly, many problems remain. When they first started to tackle the basic issues in nursing care, the nursing managers experimented with the Toyota “A3” format for problem solving. Now, they are trying to apply the same process to more involved problems such as germ routes through the wards, targeting particularly MSRAs.
Falls also remain a difficult problem, as the nurses try to encourage physiotherapy patients to greater autonomy. Difficult problems will not be solved overnight, but progress continues. Oddly enough the two greatest hindrances in this hospital to the lean approach have been the other improvement drive, such as a nationwide quality accreditation audit and a change of computer system.
In both cases, the time demands imposed on the teams with meetings, classroom training and paperwork was such that the basic discipline started to slip, and it became painfully obvious that chaos calls chaos, and that small problems, if not caught right away, can easily turn into disasters in environments as demanding as healthcare.
For the nursing manager, the greatest satisfaction of having done all this hard work is that she feels that the relationship between nursing staff and patients has noticeably improved. The environment is much calmer, people are more focused on what they need to do, and consequently, they are also far more attentive to patient demands.
On the other hand, patients are reassured by the quick response they get to their requests, and by the general aspect of an environment “that works”. In this instance, the lean approach has not relied on mapping processes, or conducting kaizen workshops.
The nursing management has tackled basic stability first and foremost, first in the environment and then in working standards. All are aware that many concerns remain. They have only recently started to look into the patient journey, and try to simplify it.
Also, they are still working on a weekly delivery cycle, and are aware they need to go to more frequent deliveries in the wards, and so on. Still, by using lean to create a learning environment, they are now in a position to learn from more advanced lean principles.
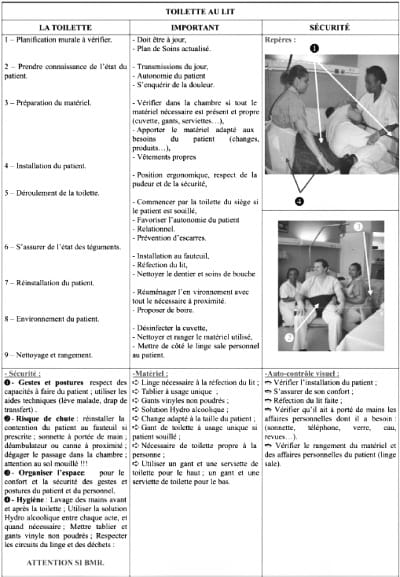
FIG. 2: Nursing standards
Ultimately, it is all about people, and processes improve when individual employees learn to do the same job better.
In his seminal paper about applying lean to healthcare, Steven J. Spear points out that “unless everyone is completely clear about the tasks that must be done, exactly who should be doing them, and just how they should be performed, the potential for error will always be high” (Spear, 2005).
Indeed, he argues that lean applied to healthcare should be essentially about creating a culture of “no ambiguity” and resolving problems through quick experimentation. The question is how to move traditional work cultures towards this lean spirit.
Traditionally, people have tried to take the lean tools developed by Toyota in automotive factories and apply them to themselves; In many cases this works in the short term, but does not actually affect the workplace culture.
In this two year experiment at Nord 92, we have tried to work through all the levels of lean, using the tools of course, but equally understanding the “system” dimension in order to promote true lean thinking: creating a working environment where all employees can visualize problems easily and find countermeasures immediately to solve them.
Nord 92’s example in using lean to carefully build a learning environment for staff and management has implications for nursing practice, certainly, but also more generally for lean implementation at large. Ultimately, as the Toyota veterans are fond of saying, lean is about “making people before making parts,” or in the wards’ context, developing nurses before delivering care.
References+ View more
- Ballé, M. and Champion-Daviller, M.-N. (2004), Organiser les services de soin: le management par la qualite´, Masson, Paris.
- Ballé, M., Beauvallet, G., Smalley, A. and Sobek, D. (2006), “The thinking production system”, Reflections, Vol. 7 No. 2, pp. 1-12.
- Jones, D. and Mitchell, A. (2006), Lean Thinking for the NHS, NHS Confederation, London.
- Spear, S.J. (2005), “Fixing health care from the inside, today”, Harvard Business Review, Vol. 83 No. 9, pp. 78-91.
References
- Ballé, M. and Champion-Daviller, M.-N. (2004), Organiser les services de soin: le management par la qualite´, Masson, Paris.
- Ballé, M., Beauvallet, G., Smalley, A. and Sobek, D. (2006), “The thinking production system”, Reflections, Vol. 7 No. 2, pp. 1-12.
- Jones, D. and Mitchell, A. (2006), Lean Thinking for the NHS, NHS Confederation, London.
- Spear, S.J. (2005), “Fixing health care from the inside, today”, Harvard Business Review, Vol. 83 No. 9, pp. 78-91.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info.
Acute care testing handbook
Get the acute care testing handbook
Your practical guide to critical parameters in acute care testing.
Download nowScientific webinars
Check out the list of webinars
Radiometer and acutecaretesting.org present free educational webinars on topics surrounding acute care testing presented by international experts.
Go to webinars








