Printed from acutecaretesting.org
April 2012
C-reactive protein point-of-care testing for respiratory-tract infections in primary care
RESPIRATORY-TRACT INFECTIONS AND ANTIBIOTICS IN PRIMARY CARE
Most oral antibiotics are prescribed in primary care [1]. Of these, the majority is prescribed to patients consulting for common respiratory-tract infections (RTI). In general, antibiotics overprescribing for lower-respiratory-tract infections (LRTI) in primary care can broadly be related to two distinct factors within the RTI consultation:
- Clinicians’ diagnostic uncertainty in differentiating serious from self-limiting disease
- Patient-related factors during the time-pressured RTI consultation.
Differentiating self-limiting from serious respiratory infections is challenging in primary care. While most respiratory-tract infections are self-limiting, some are potentially life-threatening, such as cases of pneumonia, which constitute a small but clinically meaningful part of all lower-respiratory-tract infections in primary care.
However, acute bronchitis accounts for most LRTI episodes, which is usually self-limiting. Accurately differentiating pneumonia from acute bronchitis based on clinical findings from medical history and physical examination is next to impossible, with a large discrepancy between clinical findings and radiographic pneumonia [2-4].
The supposed gold standard for diagnosing pneumonia, chest X-rays, are not routinely used in primary care for economic and logistic reasons [5]. Furthermore, radiographic examination of chest X-rays in LRTI patients from primary care shows considerable variation, questioning its reliability [6].
The superior gold standard, high-resolution computed tomography, is far from feasible in primary care LRTI patients [7]. However, in the light of possible pneumonia and with no readily available diagnostic test to rule out this condition, many family physicians (FPs) empirically prescribe antibiotics to most LRTI patients, both for pneumonia and acute bronchitis.
Several studies have indicated that to practicing FPs the needs of individuals with potential infections and maintaining good relationships with patients outweigh the perceived risk of bacterial resistance [8-10]. Yet despite this, many FPs do acknowledge that many prescriptions are unnecessary [11] and admit feeling uncomfortable in that particular situation [10].
Treatment recommendations in guidelines are mainly based on clinical diagnoses [12]. Yet with the obvious inability to accurately make these diagnoses in primary care, recommendations are hard to follow. Everyday decisions about when to prescribe antibiotics for LRTI constitute a significant part of the burden of antibiotics use that drives antibiotics resistance [13]. The use of ancillary diagnostic tests at the point of care may facilitate the diagnostic process.
This paper will focus on the use of C-reactive protein point-of-care testing for RTI based on studies performed in primary care.
C-REACTIVE PROTEIN POINT-OF-CARE TESTING FOR RTI IN PRIMARY CARE
C-reactive protein, originally named for its capacity to precipitate the C-polysaccharide of Streptococcus pneumoniae, was the first acute-phase protein to be described [14].
The acute-phase response comprises the non-specific physiological and biochemical response to most forms of tissue damage, infection and inflammation [15]. C-reactive protein is a widely used and acknowledged marker to diagnose and monitor infections in secondary care. With the emergence of point-of-care devices in the 1980s Melbye et al. were the first to evaluate the diagnostic value of the test in LRTI in primary care [16].
Unfortunately, the widespread introduction of point-of-care CRP testing in the Scandinavian countries was not accompanied by appropriate training for clinicians. Hence, in some settings this has sometimes led to an overuse of CRP testing in mostly mild respiratory-tract infections, often followed by an unnecessary antibiotics course [17, 18].
Robustness of the CRP point-of-care tests is now firmly established with studies showing reliability and accuracy of test results obtained from point-of-care devices when compared to laboratory standards [19-21].
Diagnostic studies supporting its role as an additional diagnostic marker in LRTI gradually also emerged [3, 22, 23]. A systematic review of the diagnostic role of CRP in LRTI in primary care showed that CRP was a strong predictor in differentiating pneumonia from acute bronchitis [24].
Several barriers have been mentioned for the implementation of CRP as part of routine diagnostic work-up in LRTI, including the hesitation of FPs to alter existing clinical procedures and the absence of strong randomized evidence that using point-of-care CRP could decrease antibiotics prescribing.
Secondary-care clinicians could argue that an additional diagnostic test should differentiate between bacterial and viral infections. Yet, based on large etiological LRTI cohorts we know that causative organisms can only be found in the minority of RTI cases in primary care [2, 3].
So although this aim holds for targeting appropriate antibiotics treatment in secondary care, a diagnostic test in primary care should not necessarily differentiate between bacterial and viral origin of the RTI.
The ultimate aim of such a test would be to assist FPs to differentiate serious from self-limiting infections and, as a result, assist them in withholding antibiotics in the group of patients with the latter.
EVIDENCE ON CRP POINT-OF-CARE TESTING FOR RTI IN PRIMARY CARE
Two trials investigating the effect of CRP point-of-care testing in primary care were recently performed in the Netherlands. The first involved 40 FPs and 431 LRTI patients [25].
FPs in the CRP point-of-care-test group prescribed significantly fewer antibiotics than those in the no-test group (31 % vs 53 %, P=0.02). Similarly, FPs in a group of FPs specifically trained in enhanced communication skills prescribed significantly fewer antibiotics than those in the no-training group (27 % vs 54 %, P<0.01).
Both interventions showed a statistically significant effect on antibiotics prescribing at any point during the 28-day follow-up. Clinicians in the combined-intervention group prescribed antibiotics to only 23 % of patients, while the usual-care FPs did so in 68 %.
Crucially, patients’ recovery, satisfaction with care and enablement were similar in all study groups. The interventions proved cost-effective [26].
FPs in the first trial expressed difficulties in dealing with intermediately elevated test results (20-100 mg/L) and explaining these to their patients [27], and intermediately elevated CRP results were independently associated with re-consultation [28].
Therefore, it was investigated if delayed prescriptions could be a suitable prescribing strategy for these patients, in LRTI as well as rhinosinusitis patients. The second trial involved 31 FPs and 258 patients with LRTI or rhinosinusitis. The effect of CRP assistance in antibiotics-prescribing strategies – including delayed prescribing – in LRTI and rhinosinusitis consultations in primary care was studied [29].
Patients in the CRP-assisted group used less antibiotics (43.4 %) than control patients (56.6 %) following index consultation (p=0.03). This difference remained significant during follow-up (52.7 % vs 65.1 %, p=0.04). Delayed prescriptions in the CRP-assisted group were only filled in a minority of cases (23 % vs 72 % in control group, p<0.001).
Recovery was similar across groups. Satisfaction with care was higher in patients managed with CRP assistance (p<0.05).
PRACTICAL IMPLICATIONS
Decreasing physician diagnostic uncertainty
The major contribution of CRP point-of-care testing seems to be in decreasing physician uncertainty. In particular, a CRP test result adds useful information that helps identifying those patients not at risk of a complicated illness course. We observed the greatest antibiotics reduction in patients with CRP under 20 mg/L.
This is clinically relevant, as most patients consulting in primary care will have CRP values less than 20 mg/L. Therefore, most can be gained in this specific group when withholding antibiotics treatment in those patients with CRP under 20 mg/L, albeit while considering the full clinical presentation and illness duration.
Other studies have found similar opportunities for restrictive prescribing in this group with low CRP values [30, 31].
Hence, the greatest value of CRP point-of-care testing lies in ruling out serious disease, which is a key task of FPs on a daily basis.
This brings us to a crucial role of CRP testing in primary care; the test needs to differentiate serious from self-limiting illness. This is how FPs succeeded in decreasing antibiotics prescribing. A CRP test cannot be used as a stand-alone diagnostic test for pneumonia [24].
CRP, as all other biochemical tests, should always be used within the clinical context of the particular patient. We know that individual signs and symptoms have poor operating characteristics as diagnostic tests, but in combination they are much more useful [32].
Body temperature, for instance, has poor operating characteristics as a stand-alone diagnostic test for pneumonia, but clinicians always include a consideration of temperature in the overall assessment of LRTI patients as it provides additional information.
The indications for CRP testing would be as an aid to identify patients with antibiotics-responsive serious illness and subsequently to withhold antibiotics in the large remaining group of patients with self-limiting illness. So in a way CRP in RTI is as much a prognostic marker, as it is a diagnostic marker.
DECREASING PATIENT UNCERTAINTY AND PROVIDING REASSURANCE
Additionally, CRP point-of-care testing had a role in convincing patients to accept a non-antibiotics management strategy. This was an often-mentioned advantage of CRP by FPs with experience of using the test, thereby also impacting the illness perspective of the patient [5].
Just as much as patient satisfaction with care is linked to physical examination [33], the same may apply for CRP in relation to reassurance. When investigating CRP as an additional test on top of routine consultations, those patients managed with CRP were more satisfied with the consultation compared to those managed without the test, albeit all patients showing relatively high overall satisfaction with care [29].
Additionally, CRP point-of-care testing had a role in convincing patients to accept a non-antibiotics management strategy. This was an often-mentioned advantage of CRP by FPs with experience of using the test, thereby also impacting the illness perspective of the patient [5].
Just as much as patient satisfaction with care is linked to physical examination [33], the same may apply for CRP in relation to reassurance. When investigating CRP as an additional test on top of routine consultations, those patients managed with CRP were more satisfied with the consultation compared to those managed without the test, albeit all patients showing relatively high overall satisfaction with care [29].
CUT-OFF VALUES AND AMBIGUOUS TEST RESULTS
Based on the experiences in trials and daily practice the use of cut-off values in Table I can be recommended.
TABLE I: Recommendations based on CRP* levels
|
CRP range |
Recommendation |
|
≤20 mg/L |
Self-limiting RTI Withhold antibiotics |
|
21-50 mg/L |
Majority of patients have self-limiting RTI Assessment of signs, symptoms and risk factors and CRP is important Withhold antibiotics in most cases |
|
51-99 mg/L |
Assessment of signs, symptoms, illness duration and risk factors and CRP is crucial Consider (delayed) antibiotics in high illness severity |
|
≥ 100 mg/L |
Severe infection Prescribe antibiotics |
In primary care approximately 75 % of LRTI patients will have a CRP <20 mg/L, while 5 % will have a CRP >100 mg/L. The remaining 20 % will have an intermediately elevated result (21-99 mg/L).
These intermediately elevated test results proved difficult for FPs, and their occurrence was independently associated with patient-initiated re-consultation. This association was not found when those test results were recommended to be followed by a delayed prescription. Strikingly, only the minority of patients managed with CRP filled their delayed prescription, versus the majority in the control group.
Besides the fact that the delayed prescriptions in the CRP group were better targeted at intermediately elevated results, this interesting difference can also be explained by the reassuring role of CRP and the explanation of the FP why a delayed prescription is handed out for that specific clinical presentation with associated CRP level.
COMPARISON WITH OTHER BIOMARKERS
Other potential biomarkers to differentiate serious from self-limiting infection, such as procalcitonin and lipopolysaccharide-binding protein, have somewhat less diagnostic accuracies in LRTI in primary care [34, 35].
For the former there is also evidence that it can reduce antibiotics prescribing, yet it is currently not available as a point-of-care test for primary care, and costs are considerable [36].
These constitute two essential barriers for cost-effective use of this biomarker in common infections in primary care. So at present, CRP is the most promising and cost-effective biomarker to make a difference in primary care RTIs at present.
CONCLUSION
The use of CRP point-of-care testing in RTI in primary care should only be advocated in LRTI and rhinosinusitis, and it should only be used:
- when seeking additional diagnostic or prognostic information
- to ensure further patient reassurance
The use is illustrated in Fig. 1.
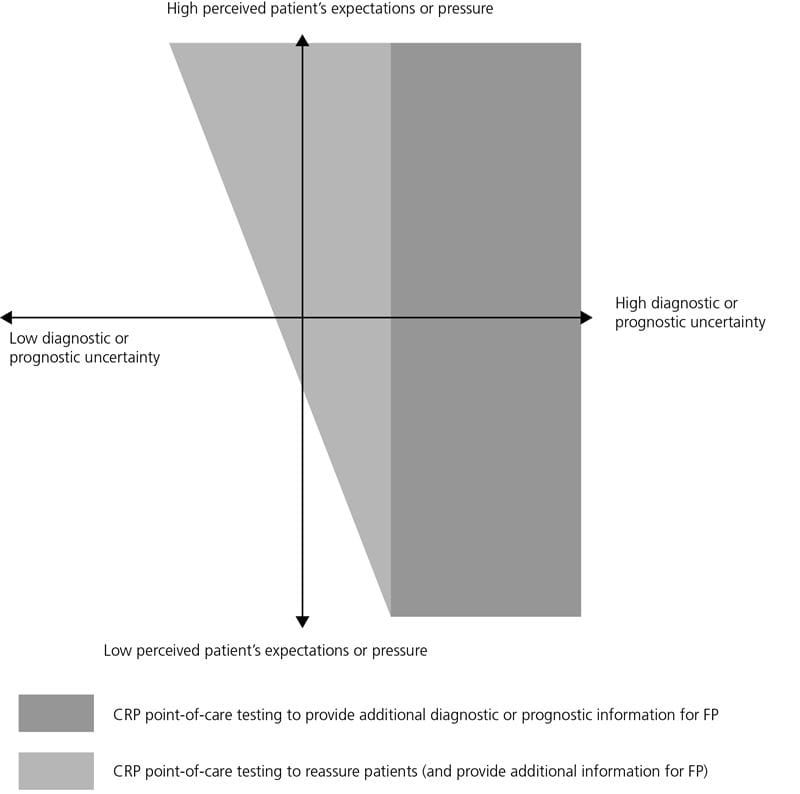
FIG. 1: Use of CRP in RTI patients
References+ View more
References
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info.
Acute care testing handbook
Get the acute care testing handbook
Your practical guide to critical parameters in acute care testing.
Download nowScientific webinars
Check out the list of webinars
Radiometer and acutecaretesting.org present free educational webinars on topics surrounding acute care testing presented by international experts.
Go to webinars








