Printed from acutecaretesting.org
April 2006
Systemwide implementation of glycemic control
Studies have been conducted to determine the impact of hyperglycemia on patient outcomes. In patients with critical illness, hyperglycemia has been associated with increased rates of sternal wound infections, hospital-acquired and surgical-site infections, increased mortality rate and other important complications associated with myocardial infarction and stroke [1-5].
Other studies have focused on the impact of tight glycemic control (TGC) on patient outcomes in diverse patient populations. Results have been astounding in the role of BG control in critically ill patients.
Implementing IV insulin therapy early and rigorously has demonstrated a reduction in morbidity and mortality and complications, including reduced length of time the patient is on ventilator support, reductions in renal failure, blood stream infections and consequences of the inflammatory process brought on by exposure to hyperglycemia [3,6-10].
Clinical strategies to maintain a euglycemic state during critical illness involve frequent monitoring for BG and implementing intravenous (IV) insulin infusions to control BG within strict parameters. Many and varied glycemic control protocols are used to maintain BG to normoglycemic levels.
However, the two variables that are common in all protocols are frequent (hourly or less) BG measurements and careful titration of IV insulin dosing to achieve BG levels within a specified target range.
This process is done to achieve targeted BG levels in the shortest time possible in a safe manner in order to limit the time of exposure of the patient to hyperglycemia. Initial and subsequent point-of-care measures of BG depend on the patient’s response to therapy and are crucial for glycemic control and detection of hypoglycemia [11-13].
Strategies for glycemic control include increased monitoring for BG in patient situations where hyperglycemia poses a threat.
Examples include patients who were critically ill, high-risk surgical patients, those with acute cardiovascular disorders, and the use of drugs that cause hyperglycemia, such as catecholamine infusions and steroid administration.
More protocols involve hourly monitoring and titration of intravenous insulin to a desired target BG. Studies on implementation of such clinical protocols to reduce BG to normoglycemic range has resulted in improved outcomes and reduced complications.
Many protocols have incorporated targets for BG within normal range (80-110 mg/dL), where others may target ranges up to 150 mg/dL, depending on patient diagnosis and maturity of the unit in glycemic control strategies and resources available.
Some protocol target ranges depend on the acuity of the patients or their location in the hospital, such as step-down monitored units or general medical/surgical wards, where less time and resources are available for hourly monitoring and the ability to titrate IV insulin.
In our organization, we began IV insulin infusions in the critical care areas first, pilot tested them, and refined the process before implementing them in specific step-down units and other hospitals within our organization.
Each step of implementation was carefully planned and rolled out in a specific manner, mostly for patient-safety concerns and adoption within the unit culture.
DEVELOPING A PERFORMANCE IMPROVEMENT PROJECT FOR GLYCEMIC CONTROL
At our institution, we recognized that we had issues with glycemic control. In December 2003, a multidisciplinary team was assembled of all major players and areas of the hospital where glycemic control was important.
Examples of disciplines and roles of team members included nurses, point-of-care-testing laboratory coordinator, physicians, certified diabetes educators, pharmacists, nutritionists, educators, administrators and unit representatives.
An initial meeting was developed to determine opportunities for improvement and develop strategies to improve performance in glycemic control. The team developed an acronym for the group so that activities for initiatives of the project were recognizable: The Systemwide Undertaking for Glycemic Achievable Results (SUGAR).
ASSESMENT OF THE PROBLEM BY THE SUGAR TEAM
Hyperglycemia was rampant and common in many patient populations at the facility. The open-heart surgery unit (CVRR) was the only unit that had clinical strategies for glycemic control. The CVRR had been an early adopter of IV insulin infusions for TGC since 1998. While the nurses in CVRR were accustomed to glycemic control and IV insulin infusion, the protocol had not been updated in years and needed further revisions to current standards.
The other intensive care units (ICUs) and the coronary care unit (CCU) had not adopted any formal initiatives toward GC. The hospitalwide physician orders for intermittent subcutaneous sliding-scale insulin were also outdated and needed revisions to include the use of long-acting, basal insulin and the incorporation of rapid acting, analog insulin.
The existing protocols had proven less than ideal in their effectiveness, and in many cases hyperglycemia was present with common measurements greater than 200 mg/dL for long periods of time. The institution did not have a policy or strategy to manage patients on insulin pumps, particularly during operative or procedural events.
Education of nurses in the organization was variable, and with the advent of many new insulin and oral glycemic control medications, development of standardized and updated education was needed to avoid errors in insulin administration.
Additionally, turnover of nursing staff, high numbers of nursing students and physician residents, and use of agency personnel yielded new groups of professionals entering the organization who required introduction to new glycemic control standards.
The SUGAR team established small working groups to develop specific changes in practice with clear timelines for dissemination throughout the organization. The key areas determined by the team for development were establishment of clear guidelines and protocols for glycemic control, multidisciplinary/multiprofessional education, and patient education.
BEST-PRACTICE DEVELOPMENT BY THE SUGAR PROJECT
The SUGAR team reviewed all areas for improvement and prioritized their development. A uniform approach was designed to address elements needed for successful implementation: protocol and guideline development, education and strategies for pilot testing in a few units, followed by systemwide dissemination. Development teams were assimilated for each specific initiative. Since the project began, the following best-practice designs were accomplished:
- Hypoglycemia protocols, guidelines and education for adults and pediatrics
- IV insulin order set for critical care, guidelines and education for adults
- Subcutaneous insulin regimen for adults, education
- Policy and procedures and guidelines for glycemic control with insulin pump
- Uncontrolled diabetic states: diabetic ketoacidosis and hyperglycemic hyperosmolar syndrome order sets, guidelines and education
The reason for this approach was to streamline and provide a standard approach based upon the best scientific evidence available and to reduce variation in practice related to glycemic control. Each of these strategies for glycemic control was implemented in a systematic manner, driven by advanced practice nurses, physicians and nurse educators in specific practice areas.
All of these initiatives required presentation to appropriate committee meetings such that everyone was on board with the new initiatives, including specific practice committee groups, pharmacotherapy and therapeutics, physician leadership groups and collaborative practice teams. This involvement from key leaders in each area of practice was essential for buy-in and adoption of new strategies.
Educational programs were developed for each guideline and were made available to all areas of practice. A specific website for the SUGAR project and online education was established to facilitate the education process on each initiative.
The educational offerings included slide presentations, a posttest, and any associated order sets, protocols, references or guidelines on each topic. These programs were made mandatory for all nurses in the acute care setting where the content applied to their area of practice.
IMPLEMENTING TGC INITIATIVES
During the implementation phase, active presence was required to reinforce IV insulin protocols. This included active involvement of physicians, pharmacists, advanced practice nurses and educators to guide staff through the new protocol during the adjustment and education phases.
This was extremely important for successful implementation as the IV insulin physician order sets were complex and required guidance until fully adopted by staff. This strategy was also important for patient safety to make sure the elements are followed and for efficacy of dosing for glycemic control.
We encountered some resistance from nurses and physicians on adopting tight glycemic control practices. They had voiced concern over putting the patient at risk when putting the patient on IV insulin to lower control levels and frequent finger sticks for hourly monitoring.
Over time, however, clinicians were able to appreciate the success of the infusion orders in controlling BG without adverse side effects and acquired mastery of using the protocol, and the initial resistance has diminished.
MONITORING FOR SAFETY AND EFFECTIVENESS
Several focus studies have been done during implementation of the glycemic control initiatives with the SUGAR project in the critical care units prospectively. We studied the impact of our IV insulin infusion orders on reaching BG target range, compliance with the protocol, and hypoglycemic events [14].
This was possible through coordination with the point-of-care-testing coordinator to receive reports and data to evaluate BG monitoring patterns and blood glucose results. As a result, we could determine the impact of IV insulin on the number of tests performed during the study period. After these studies were complete, we were able to revise the IV insulin orders consistent with our findings.
An additional study was conducted on the nursing work involved, perceptions on frequent BG monitoring and titration of insulin therapy, and approximate costs, and was able to evaluate the impact on average blood glucose values from the units over time [15-16].
In this study, we found that while nurses believed that glycemic control was important, the work effort required was extensive and cumbersome. Estimated costs associated with glycemic control over a 1-year period in the intensive care units alone approximated USD 250,000.
Nursing time spent on glycemic control alone averaged approximately 2 hours of direct patient care time. Recommendations from this study were to find new ways of BG monitoring, such as automated systems and non-invasive monitoring.
At present, new strategies are being developed for glycemic control and by industry to develop such devices and will have a potential impact on glycemic control in the future [17-18]. We also realized that we needed more point-of-care BG monitoring machines in each unit to accommodate increases in BG monitoring with IV insulin infusion.
Part of monitoring the impact of the SUGAR project involved coordination with the pharmacist in charge of recording medication errors. The team started receiving reports of medication errors related to glycemic control and insulin administration. These were reported in leadership meetings, and ways to improve patient safety in glycemic control were addressed.
CONTINUED AND SUSTAINED AWARENESS AND EDUCATION ON GLYCEMIC CONTROL
Throughout the initiative, an increased awareness of the importance of glycemic control was established by grand rounds presentations for nurses, physicians, pharmacists and other multidisciplinary groups.
The SUGAR project initiatives and results of focused studies were made public in all relevant committees and administrative groups. Unit education was conducted where glycemic control strategies were being adopted and a new computer-assisted program for glycemic control is being developed for systemwide access to education.
The SUGAR team also posted results of the pilot tests for safety and efficacy for wide dissemination to all staff.
Currently, all new nurses hired in the organization, including student nurses and their educators, are required to complete the SUGAR education as part of their orientation to our system.
We are developing strategies for unit designation for acute diabetes states and management, with highly specialized education for all staff (physicians, nurses, clinical technicians) for highly specialized care in glycemic control.
Patient education programs have also been implemented to address the need for continued education for patients with diabetes and newly diagnosed cases of diabetes. All of the glycemic control initiatives are being disseminated to all the hospitals within the organization using the same methods that were successful at the initial site of implementation.
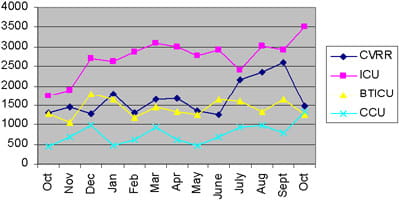
FIGURE 1: Critical Care Units - Number of POCT BG
tests
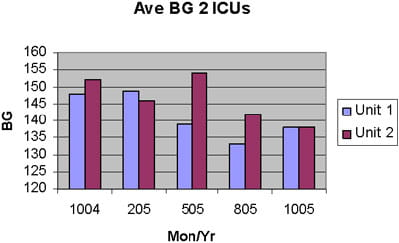
FIGURE 2: BG over time
SUMMARY
In summary, glycemic control is a multidisciplinary, multiprofessional process. Safe and effective means for glycemic control requires developing a strategic plan by an organization with a systemwide approach to glycemic control with the common goal of improving patient care and outcomes.
Involvement of key team players and leaders are essential for successful implementation of glycemic control strategies.
References+ View more
- Capes SE, Hunt D, Malmberg K, et al. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients. Stroke 2001; 32: 2426-32.
- Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet 2000; Mar 4; 355: 773-78.
- Furnary AP, Zerr KJ, Grunkemeier GL, Starr A. Continuous IV insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg 1999; 67(2): 352-60.
- Aragon D, Ring C, Covelli M. The influence of diabetes mellitus on postoperative infections. Crit Care Nurs Clin 2003; 15(1): 125-35.
- Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc 2003; 78: 1471-78.
- Grey NJU, Perdrizet GA. Reduction of nosocomial infections in the surgical intensive-care unit by strict glycemic control. Endocrine Prac 2004; 10(Suppl 2) March/April: 46-52.
- Furnary AP, Guangqiang G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac and Cardiovas Surg 2003; 123(5): 1007-21.
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. NEJM 2001; 345(19): 1359-67.
- Krinsley JS. Effect of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc 2004; 79(8): 992-1000.
- Pittas AG, Siegel RD, Lau J. Insulin therapy for critically ill hospitalized patients: A meta-analysis of randomized controlled trials. Arch Intern Med 2004; 164: 2005-11.
- Quevedo SF, Sullivan E, Kington R, et al. Improving diabetes care in the hospital using guideline-directed orders. Diabetes Spectrum 2004; 14(4): 226-33.
- Goldberg PA, Siegel MD, Sherwin RS, et al. Implementation of a safe and effective insulin infusion protocol in a medical intensive care unit. Diabetes Care 2004; 27(2): 461-67.
- Zimmerman CR, Mlynarek ME, Jordan JA, et al. An insulin infusion protocol in critically ill cardiothoracic surgery patients. Ann Pharmacother 2004; 38: 1123-29;
- Dillard C, Aragon D. Implementation of an insulin infusion order set: The SUGAR Project. Clin Nurs Specialist 2005; 19(3): 157.
- Aragon D. Evaluation of nursing work effort and perceptions about blood glucose testing in tight glycemic control. Crit Care Med 2005, (suppl) 33(12): A13.
- Aragon D. Evaluation of nursing work effort and perceptions about blood glucose testing in tight glycemic control. Amer J Crit Care (accepted manuscript for publication 2006 – in press)
- Bland DK, Fankhanel Y, Langford E, et al. Intensive verses modified control of blood glucose level in medical intensive care patients: A pilot study. Amer J Crit Care 2005; 14(5): 370-76.
- Goldberg PA, Siegel MD, Russell RR, et al. Experience with the continuous glucose monitoring system in a medical intensive care unit. Diabetes Technol Ther 2004; 6(3): 339-47.
References
- Capes SE, Hunt D, Malmberg K, et al. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients. Stroke 2001; 32: 2426-32.
- Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet 2000; Mar 4; 355: 773-78.
- Furnary AP, Zerr KJ, Grunkemeier GL, Starr A. Continuous IV insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg 1999; 67(2): 352-60.
- Aragon D, Ring C, Covelli M. The influence of diabetes mellitus on postoperative infections. Crit Care Nurs Clin 2003; 15(1): 125-35.
- Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc 2003; 78: 1471-78.
- Grey NJU, Perdrizet GA. Reduction of nosocomial infections in the surgical intensive-care unit by strict glycemic control. Endocrine Prac 2004; 10(Suppl 2) March/April: 46-52.
- Furnary AP, Guangqiang G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac and Cardiovas Surg 2003; 123(5): 1007-21.
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. NEJM 2001; 345(19): 1359-67.
- Krinsley JS. Effect of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc 2004; 79(8): 992-1000.
- Pittas AG, Siegel RD, Lau J. Insulin therapy for critically ill hospitalized patients: A meta-analysis of randomized controlled trials. Arch Intern Med 2004; 164: 2005-11.
- Quevedo SF, Sullivan E, Kington R, et al. Improving diabetes care in the hospital using guideline-directed orders. Diabetes Spectrum 2004; 14(4): 226-33.
- Goldberg PA, Siegel MD, Sherwin RS, et al. Implementation of a safe and effective insulin infusion protocol in a medical intensive care unit. Diabetes Care 2004; 27(2): 461-67.
- Zimmerman CR, Mlynarek ME, Jordan JA, et al. An insulin infusion protocol in critically ill cardiothoracic surgery patients. Ann Pharmacother 2004; 38: 1123-29;
- Dillard C, Aragon D. Implementation of an insulin infusion order set: The SUGAR Project. Clin Nurs Specialist 2005; 19(3): 157.
- Aragon D. Evaluation of nursing work effort and perceptions about blood glucose testing in tight glycemic control. Crit Care Med 2005, (suppl) 33(12): A13.
- Aragon D. Evaluation of nursing work effort and perceptions about blood glucose testing in tight glycemic control. Amer J Crit Care (accepted manuscript for publication 2006 – in press)
- Bland DK, Fankhanel Y, Langford E, et al. Intensive verses modified control of blood glucose level in medical intensive care patients: A pilot study. Amer J Crit Care 2005; 14(5): 370-76.
- Goldberg PA, Siegel MD, Russell RR, et al. Experience with the continuous glucose monitoring system in a medical intensive care unit. Diabetes Technol Ther 2004; 6(3): 339-47.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info.
Acute care testing handbook
Get the acute care testing handbook
Your practical guide to critical parameters in acute care testing.
Download nowScientific webinars
Check out the list of webinars
Radiometer and acutecaretesting.org present free educational webinars on topics surrounding acute care testing presented by international experts.
Go to webinars








