Printed from acutecaretesting.org
April 2015
Update on Procalcitonin Measurements
PROCALCITONIN (PCT) AS A MARKER FOR THE DIAGNOSIS OF SEPSIS AND TO GUIDE ANTIBIOTIC THERAPY
PCT has the highest accuracy for the diagnosis of sepsis in various settings. The lag time for PCT induction is approximately 2 to 4 hr after the onset of sepsis, a time period that has usually passed if patients are presented at the emergency department (ED).
Peak levels of PCT occur at 24 to 48 hr after sepsis. Early treatment of sepsis is most effective ("the golden hours of treatment"), and complications like organ dysfunction indicate an already progressed state of the disease.
Therefore, early confirmation of systemic inflammation and sepsis, as done by PCT measurement, is most important. Various studies have confirmed that survival rate of patients with sepsis can be significantly improved if antibiotic therapy is initiated immediately using the right antibiotics [1].
Point-of-care (POC) tests, despite being semi-quantitative, are helpful in situations when quantitative measurements are not going to be available within reasonable time (1-3 hr).
However, a semi-quantitative POC test should be sensitive enough to indicate or exclude systemic inflammation. This usually requires a lower assay sensitivity of 0.2-0.3 ng/mL. If the clinical impression indicates a possible diagnosis of sepsis, but PCT levels are not elevated, patients should still be treated for sepsis initially, regardless of the high negative predictive value of normal PCT.
Monitoring patients during the next one to two days will indicate whether the initial diagnosis is correct and antibiotics can be discontinued early if sepsis is excluded and PCT remains low. This approach is also supported by the society of critical care medicine (SCCM) sepsis guidelines [2]. PCT is also a food and drug administration (FDA)-approved diagnostic marker.
PCT has also proved to be useful in guiding antibiotic therapy. This approach was mainly evaluated in patients with respiratory tract infections; however, it can also be used in critically ill patients with sepsis or severe sepsis of various origins [3-7].
In addition, in outpatients with respiratory tract infection and exacerbation of chronic obstructive pulmonary disease (COPD), antibiotic prescription rates were significantly reduced by the use of PCT [8, 9]. This diagnostic approach is also recommended in various guidelines [10, 11].
INDUCTION AND BIOCHEMICAL PROPERTIES
PCT was described as a marker of sepsis in 1993 [12]. It is a soluble protein liberated into the circulation of patients in response to severe systemic inflammation, in particular by bacterial infection.
Biochemically, it is the prohormone of the hormone calcitonin, but the biological function and induction are different from that of calcitonin. The induction of PCT is more strictly regulated as compared to cytokines: there is no significant PCT production in stimulated whole blood, but PCT production has been observed in various tissues during sepsis.
The induction of circulating PCT is related to the activation and adherence of monocytic cells, which occurs during sepsis as well as in other conditions such as after tissue trauma. Adherent monocytes and adipocytes, when in contact with activated monocytes, have been shown to produce PCT ex vivo [13].
The role of liver during PCT induction has been demonstrated in a baboon endotoxin shock model, in which the PCT response was significantly attenuated after liver explantation [14]. This difference in regulation of induction may be one reason why PCT has a different profile than other markers of sepsis.
Diagnostic tests measure the calcitonin/N-ProCT part of the protein and hence only a fragment of the 114-116 amino acid chain of the prohormone. Plasma levels of PCT in healthy individuals are quite low (<0.1 ng/mL) [15].
To exclude sepsis and systemic inflammation, a concentration of ≤0.2 ng/mL is a useful reference range. As a cut-off for the diagnosis of sepsis, plasma levels of ≥0.5 ng/mL are interpreted as abnormal and suggest sepsis.
After reaching peak levels, the circulating PCT concentration declines with a 50% plasma-disappearance rate of roughly 1-1½ days. In patients with severe renal dysfunction, elimination rates may be prolonged (one third to one half), but accumulation of PCT does not occur.
Various biological functions of PCT have been described. These include modulation of immunologic functions and vasomotility. Some effects are time-dependent and different in normal and prestimulated cells.
For example, the migratory response of monocytic cells is augmented by PCT, but it gets inhibited after some hours of incubation with PCT [15]. Similarly, expression of inducible nitric oxide synthase (iNOS) in vascular smooth muscle cells is inhibited by PCT in native cells, but it is augmented in prestimulated cells [16, 17]. In addition, PCT has been shown to influence the expression of cytokines.
In experimental shock models, neutralization or injection of PCT had an impact on the survival and organ dysfunction in the hamster and porcine animals, but injection of PCT into sham animals was found to have no effect. Hypothetically, these effects of PCT may contribute to the different local and systemic response of perfusion and inflammation of tissue observed in patients with sepsis.
COMPARISON WITH OTHER MARKERS OF SEPSIS
PCT has a different profile than other presently used markers of sepsis, such as C-reactive protein (CRP), lactate, or various proinflammatory cytokines (interleukin (IL)-6, IL-8).
It also belongs to a different class of molecules, which may be called "hormokines," as suggested by Mueller et al. [18], which indicates the cytokine-like behavior of PCT during inflammation and infection. It is also a natural substrate for dipeptidyl-peptidase IV, which inactivates various cytokines [19].
The specificity of CRP for the diagnosis of sepsis is rather low and its peak plasma levels do not indicate the severity of systemic inflammation adequately. Hence, CRP concentrations can be misleading and may fail to diagnose severe sepsis [20-22].
CRP levels may also be significantly elevated in response to various types of stimuli, such as different types of trauma and inflammation, which may not necessarily be a case of severe infection or sepsis. For example, after both minor and major surgery, CRP levels may be elevated to >50 mg/mL [23].
However, there may be only a moderate increase of CRP level (50-100 mg/L or less) in patients with an acute onset of sepsis or even severe sepsis. This may lead to inappropriate treatment due to which fatal consequences have been reported.
Finally, not only does the increase to peak levels of CRP may take several days, the decline of its increased plasma levels may also take up to one or two weeks. As a result, CRP is not considered to be a useful marker in the intensive care unit (ICU) and in critically ill patients.
Lactate is also frequently used as a biomarker for sepsis, severe sepsis, and septic shock. However, lactate is not an early indicator of sepsis and lacks specificity. It is primarily a marker of impaired oxidative metabolism or perfusion abnormalities, which may be an epiphenomenon of sepsis and organ dysfunction.
Several other conditions may also cause an increased lactate production or a decreased lactate clearance. Since perfusion abnormalities and impairment of oxidative metabolism are closely related to organ dysfunction, success of therapeutic interventions may already be limited, if lactate level has increased significantly (>4 mmol/L).
Lower levels of lactate (<2 mmol/L) are less specific and are more frequently seen in critically ill patients. In addition, lactate levels do not clearly differentiate a septic from a nonseptic shock [24].
Cytokines and various other novel and recently published markers of sepsis generally do not exhibit significant advantage over PCT measurement except for some specific features. They either do not indicate severity of systemic inflammation (e.g. the endotoxin activity assay, soluble triggering receptor expressed on myeloid cells 1 (sTREM-1), and various acute phase proteins) or the relative specificity for bacterial induced sepsis is low (e.g. cytokines).
However, cytokines react immediately to severe systemic inflammation and hence do not have the disadvantages of CRP or lactate measurements. Cytokine levels are also increased in local effusions, which is usually not seen in case of PCT. High levels are correlated with the severity of systemic inflammation and an impaired outcome (e.g. IL-6 levels >1,000 pg/mL and higher) [25, 26], but they lack specificity and peak levels may change rapidly without clinical correlation.
Despite of this, in some patients, the quick response of IL-6, in terms of both increase and decrease, may provide additional information. In addition, these biomarkers have not been consistently investigated for their role as a guide to antibiotic therapy. Only some studies investigated this topic, and this is not evidence enough for a clinical routine use [27].
During routine clinical investigations, various other laboratory markers should be observed for an unexpected diagnosis of sepsis. For example, various coagulation parameters, D-dimers, thrombocyte and leukocyte counts, and temperature may indicate an unexpected onset of sepsis. A specific diagnosis can then be confirmed using more specific markers like PCT.
DIAGNOSIS OF SEPSIS, SEVERE SEPSIS, AND SEPTIC SHOCK
High PCT levels have a high positive predictive value to rule in the diagnosis of sepsis, severe sepsis, or septic shock (PCT >0.5 to >2 ng/mL). On the contrary, normal or very low PCT plasma concentrations have a high negative predictive value to rule out severe systemic inflammation or sepsis (PCT <0.25 to <0.5 ng/mL).
These are the hallmarks of PCT diagnostics. The common link between PCT elevation and bacterial infection is the severity of systemic inflammatory response. Bacterial infection is a strong stimulus for PCT production whereas if the systemic inflammation is due to viral infection, the PCT induction is low [28-31]. Also in patients with SIRS, there may be PCT induction, but this is usually not as high as in severe sepsis.
In situations such as in patients with aneurysmal subarachnoid hemorrhage, the high negative predictive values of low PCT (<0.2 ng/mL) can be used to exclude an infection [32]. It is also important to note that various conditions other than bacterial infection may induce PCT elevation, for example, severe trauma, some autoimmune disorders, or prolonged cardiogenic shock.
On the other hand, a local bacterial infection does not induce significant amounts of PCT. In case of endocarditis, for example, PCT can be normal or elevated, depending on the systemic inflammatory response.
Similarly, PCT levels may be low, if there is no systemic inflammatory response in patients with bacteremia. However, patients with bacteremia usually have significantly high PCT levels and therefore, bacteremia is not very likely if PCT levels are found to be normal [33-35].
SEVERITY OF INFLAMMATION AND FOLLOW-UP OF TREATMENT
The severity of the systemic inflammatory response is roughly correlated with the severity of systemic inflammation, although a gold standard is missing. Usually, high PCT levels are found in patients with severe sepsis and septic shock.
The elevated as well as highly elevated level of PCT (>2 ng/mL or >10 ng/mL, respectively) is a sign of alarm indicating a high risk of organ dysfunction due to systemic inflammation and calls for immediate treatment of the patient.
Depending on the success of therapy, high PCT levels are more frequently related to an increased mortality risk. Indeed, low PCT levels were related to a better outcome in patients with sepsis and infection as well as acute pancreatitis [36-39]. Importantly, the course of PCT levels over time, rather than absolute PCT values, affect the prognosis of systemic inflammation; continuously declining PCT levels indicate a better prognosis, even if the peak PCT values are very high.
A persistent increase or failure to decline in the PCT levels has been related to higher mortality rates in various studies [40-43]. On the other hand, as a rule of the thumb, a decline of > 30% per day indicates significant improvement of systemic inflammation. This decline is consistent with the natural plasma disappearance rate of PCT [44].
LOCAL INFECTION
Local bacterial infection or bacterial colonization usually does not induce PCT (for example, tonsillitis, minor soft tissue infection, abscess, local infection of a cerebral ventricular drainage, and even local appendicitis or cholecystitis).
Hence, PCT cannot be used to diagnose (local) infection such as, infection of a cerebral ventricular drainage. In addition, this marker cannot be used as a screening tool to search for infection, if systemic inflammation is not active.
In this situation, however, the patient´s risk of dying from organ dysfunction, sepsis, or severe sepsis is very low. If clinical symptoms indicate a possible sepsis, but the PCT level is low, sepsis therapy should be started anyway, and PCT measurements should be repeated (after 12, 24, 36 hr) until the final diagnosis is clear.
PCT ELEVATION IN PATIENTS WITHOUT SEPSIS
PCT levels may be elevated in patients who do not have sepsis. Plasma levels in these cases usually are not very high (<2 ng/mL), but they may increase significantly in certain conditions, e.g. following liver transplantation, during severe and prolonged cardiogenic shock, in patients with heat shock, severe pancreatitis, and rhabdomyolysis (>2-10 ng/mL).
In addition, certain types of autoimmune disorders may induce significant amounts of PCT. Therefore, it is important that the physician, especially in the ICU, is aware of any such conditions because the sensitivity and specificity of diagnostic tests can be increased, if individual conditions of the patients are taken into account. A selection of conditions where PCT is induced independent of sepsis and infection are indicated in Table 1.
In patients with low PCT levels, antibiotic therapy should be discontinued, if damage from any putative site of infection is not expected. Whether antibiotic therapy should be withheld in neutropenic patients with fever and normal PCT levels, and in patients with acute pancreatitis and low PCT levels is still under discussion.
A low PCT level in patients with acute pancreatitis indicates that antibiotic therapy may not be required, since low PCT levels are associated with a low risk or low severity group of patients, most likely having edematous pancreatitis.
It is yet to be investigated whether PCT is an indicator of urgency for surgery in patients with minor abdominal complaints (e.g. suspected appendicitis), despite several discussions for a possible need for categorization of these patients in order to differentiate complicated cases for urgent intervention and less severe cases only requiring conservative therapy [45-50].
INDIVIDUAL, PATIENT-ADAPTED ANTIBIOTIC THERAPY USING PCT: “ANTIBIOTIC STEWARDSHIP”
PCT-guided antibiotic therapy has been investigated in various studies, which suggest that the duration of antibiotic therapy and unnecessary treatment courses can be avoided and consumption of antibiotics significantly reduced using PCT.
Hence, a PCT-guided approach should be a part of any antibiotic stewardship program to avoid overuse of antibiotics. Meanwhile, as a guide for antibiotic therapy, PCT is also mentioned in various guidelines [10, 11].
INDICATIONS
A PCT-guided approach can be used in various patients and indications, but the goal and approach may be different: i) In outpatients, unnecessary antibiotic prescriptions can be avoided because usually the main reason for prescription of antibiotics is reduction of symptoms that may actually be caused by local bacterial or viral infection.
This has been demonstrated specifically for acute respiratory tract infection and exacerbation of COPD [8, 9]. The rate of sepsis and severe infection in these patients is rare and the low cut-off for PCT (e.g. <0.25 ng/mL) provides a level of security due to the high negative predictive value of low concentrations to exclude sepsis. ii).
In critically ill patients with sepsis, severe sepsis, or severe bacterial infections like pneumonia, success of therapy and duration of antibiotic treatment can be evaluated and individually adapted by PCT measurement. Nowadays, individually adapted treatment courses should be the choice, instead of prescribing a fixed term of antibiotics.
Unfortunately, most guidelines still cover only the worst case scenario and hence favor overtreatment. iii) In the ED, diagnosis or confirmation of diagnosis of sepsis or the differential diagnosis is the main indication for PCT measurement.
High PCT levels indicate a high urgency for sepsis therapy, including a search for a focus or surgical intervention. The idea of this concept is that patients with very low or normal PCT levels have a low risk for sepsis and systemic inflammation and hence a low mortality due to severe bacterial infection, at least at the time when low PCT is measured.
Therefore, antibiotic therapy may not be required immediately and after focus removal, successful treatment courses may be discontinued based on the individual patient requirements. Further, only periods of invasive bacterial infection should be treated, rather than colonization or local superinfection.
Also, attempts of eradication of certain strains of microorganisms may have limited success and cause further selection of resistance to the microorganisms. Therefore, such attempts have limited advantage for the patient in the long term.
Exclusion criteria for the use of this concept are situations where PCT is not induced or treatment is required anyway, for example, i) in patients who have no significant PCT response, ii) patients in whom treatment of local infection is essential, e.g. those who have infection of vital organs (e.g. endocarditis, ventriculitis), iii) infection with slowly growing microorganism or tissue, toxin-producing microorganism or infections with low immunogenic responses (like osteomyelitis, tuberculosis, infection with atypical microbe, and sometimes, fungal infection), iv) patients who have severe immunosuppression or a limited ability to eliminate residual infection, and v) patients in whom the focus of infection has not been eliminated.
It is not essential to mention here that an unexpected deterioration of the disease cannot be predicted even by PCT.
TABLE I: Indications for PCT measurement other than bacterial or fungal infection
|
Condition |
Comments /Peak |
Expected range |
Reference |
|
Surgery, trauma, burn, and |
Maximum values on day 1, rapidly declining |
<0.5-1 ng/mL for peripheral, non-abdominal trauma or |
[23, 68, 69] |
|
Cardiogenic shock |
Initially low, but increasing within 1-3 days, if vasopressor |
May be intermediate to high |
[76-78] |
|
MODS, severe SIRS |
Increases with severity. |
0.5 ng/mL-2 ng/mL, rarely >10 ng/mL |
[79, 80] |
|
Pancreatitis, severe |
Low PCT indicates less severe or edematous pancreatitis. Infection not likely. |
<0.2 ng/mL: mild or edematous pancreatitis. |
[37-39, 83] |
|
Autoimmune disorders |
Induction depends on the type: |
Usually less than 0.3-0.5 ng/mL, in some types |
[84-90] |
|
Severe renal or liver dysfunction |
Chronic and moderate elevation, only at severe |
In the lower range, 0.1-2 ng/mL, constant elevation |
[44, 91-94] |
|
After prolonged resuscitation, |
Peak Day 1 |
Only In case of prolonged CPR, levels are related with |
[97, 98] |
|
Neonates after birth |
Peak Day 1-2 |
Use adapted reference range |
[99-102] |
|
End stage of tumor disease |
Slow increase. Para neoplastic induction very rare, |
Low (0.5-2 ng/mL) |
[103] |
|
Rhabdomyolysis |
Acute |
May be very high |
Individual reports |
PRACTICAL APPROACH
As demonstrated in various studies, by using PCT measurements, approximately two to three days of antibiotic consumption can be saved. For a practical approach, we recommend a daily PCT measurement in all critically ill patients from the onset of antibiotic prescription, with the following periods of interpretation: first, during day-2 to day-3 of treatment, success of therapy can be evaluated by assessing the PCT kinetic (e.g. a decline indicates a positive response to therapy).
Second, from day-3 to day-6 of treatment, one must be aware that antibiotics can be discontinued in the majority of patients at this time (see PCT guided algorithm). In our hospital, we used the algorithm by Bouadma et al. [3].
This algorithm involves both criteria of absolute PCT cut-off values and a kinetic algorithm, for either initiation or termination of antibiotic therapy (Fig. 1). The kinetic algorithm is important for the ICU, since very low cut-off values for PCT used in outpatients and the ED (0.2 ng/mL), are less frequently seen in critically ill patients even after successful focus elimination.
Third, latest at day-7- there should be a general rule to stop antibiotic therapy in all patients, unless specific requirements justify further treatment. However, this decision must be actively discussed within the team and documented in writing. Specific indications like treatment of endocarditis or severe bone infection are excluded from this rule.
Various studies indicate that a maximum duration of treatment of approximately seven days is enough to treat even a severe focus of bacterial infection or sepsis [3, 5, 6, 51, 52].
POSSIBLE SIDE EFFECTS
This concept has no obvious disadvantages for the patient and no adverse effects if used appropriately. Despite of this, there has been criticism that the statistical power to rule out significant effects on mortality may not be enough and investigations so far have mainly included patients with lower respiratory tract infections [53, 54].
Until now, more than 4,000 patients have been evaluated in randomized controlled trials. In a meta-analysis, Schuetz et al. [55] reviewed data of 4,221 patients who have been investigated in 14 trials.
The results showed that 134 out of 2,126 patients in the control groups and 118 out of 2,085 patients in the PCT-guided groups died, thus confirming the non-inferiority of PCT on a statistical level, which was equivalent to exclude an effect of PCT measurement on mortality rate below 8-10%.
In a computer-based model, retrospective data analysis from 1,312 ICU patients and an arbitrary use of PCT-algorithm showed substantial reduction in the treatment costs, based on the German DRG system (DRG, diagnosis related groups, a system of disease related reimbursement) [56].
Two minor studies in France did not see a beneficial effect of PCT based algorithm, but others confirmed the significant reduction of antibiotic use in the clinical routine as well [57, 58]. Further studies are under way, e.g. in the Netherlands that includes more than 1,800 patients [59].
However, it is important to consider that the results of such studies always depend on the training and experience of the team, the level of implementation of the method, regional features, and the patients selected [60-62].
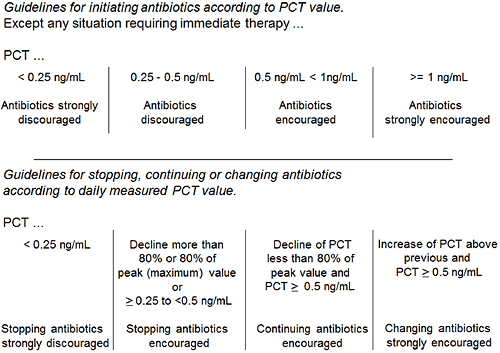
Fig. 1. Example of an algorithm for an individual guide of antibiotic therapy according to Bouadma et al. [3].
DATA OF PREVIOUS STUDIES: OUTPATIENTS AND THE ED
The group of B. Mueller, M. Briel, and P. Schütz conducted a multi-center trial in outpatients, including 458 patients for whom the treating physician initially decided to prescribe antibiotics on a routine basis, and the control group. In the treatment group, the decision was re-evaluated after presentation of the PCT-guided recommendation (no prescription if PCT <0.1 ng/mL or <0.25 ng/mL).
As a result, 72% of patients in the PCT- guided group did not get antibiotics as compared to the control group. They did not have more complications, the number of sick days was the same, and fewer side effects, such as diarrhea, were observed [8].
In patients with exacerbation of COPD, a similar PCT-guided algorithm was used [9]. In the control group (without PCT measurement), the antibiotic prescription rate was 72%, while in the PCT-guided group it was 40%. During a 6-month follow-up period, complication rates were similar in both groups (regarding mortality, hospitalization, and reinfection). Also, in this study, a low PCT cut-off value for the decision of "no antibiotics recommendation" was used (0.1 to 0.25 ng/mL).
Further studies confirmed feasibility and usefulness of this approach in outpatients and the ED in different circumstances in a higher number of patients.
In another multicenter study, where 1,759 patients were included, duration of antibiotic therapy was 1.5 days shorter in the PCT- guided group (7.4 vs. 5.9 days) [57]. For acute exacerbation of infection in patients with idiopathic pulmonary fibrosis and for treatment of patients with malignancies, reduction in the use of antibiotics with the help of PCT measurement has also been reported [63, 64].
In 243 patients, presenting in the ED with respiratory tract infections and symptoms of dyspnea and cough, prescription of antibiotics was only 44% in the PCT- guided group as compared to 83% in the controls. Primarily, patients with no bacterial infection (asthma) or a non-invasive disease (e.g. bronchitis) did not get antibiotics [65].
1. Community Acquired Pneumonia In patients with community-acquired pneumonia (CAP) (N=302), 151 patients were treated according to the recommendation of a PCT-based algorithm. Duration of antibiotic treatment was 5 days in the PCT- guided group as compared to 12 days in controls.
In patients who had a lower risk or a less severe pneumonia (pneumonia severity index PSI I-III), treatment courses were even shorter (4 days or less). In patients who had severe pneumonia or a high-risk classification (PSI IV-V), treatment courses were not longer than 7 days in the majority of patients [66].
Schuetz et al. [51] analyzed 671 patients in a PCT- guided group and 688 patients as controls. Patients had respiratory tract infections of different types and severity (CAP, eCOPD, and bronchitis).
Exposure to antibiotics was reduced approximately one third in all diagnostic groups, with an overruling rate of approximately 10% for both predefined criteria and the individual decision of the treating physicians to not obey the recommendation of the algorithm.
Adverse effects were not significantly different in both groups.
In the study by Bouadma et al. [3], 621 patients with different diagnosis were included. This study mainly included patients with lower respiratory tract infections (CAP and ventilator-associated pneumonia [VAP]), but also had some patients with abdominal and urinary tract infections.
Exposure to antibiotics was reduced by 23% in the test group as compared to the control group during the 28-day observation period.
OTHER DIAGNOSIS AND PATIENTS WITH SEPSIS
Even though patients with diagnosis other than pneumonia were underrepresented in these studies, further data indicate that a PCT-guided antibiotic stewardship can be achieved in patients with other diseases as well.
Using a similar PCT-based algorithm, 101 patients with VAP were analyzed and it was observed that the duration of therapy was 9.5 days in the PCT-guided group (51 patients) as compared to 13 days in the control group [4].
In another study, Nobre et al. [52] analyzed 68 patients with severe sepsis out of which, 31 patients were treated according to the recommendations of a PCT-guided algorithm. It was found that the duration of antibiotic treatment course was 3.5 days shorter in the PCT group as compared to the control group.
Hochreiter and Schroeder et al. [5, 6] analyzed postsurgical patients with sepsis and patients with severe sepsis, using another algorithm (PCT cut-off <1 ng/mL or decline of >30% after 3 days) and treatment duration in the PCT-guided group was 5.9 days vs. 7.9 days in control group.
A review of data from 2005 to 2009 (when the PCT-guided algorithm was introduced), indicated reduction in the duration of antibiotic courses from 14 days in 2005 to 9 days in 2009 [67].
In 71 patients with severe acute pancreatitis, a PCT-guided approach (cut-off >0.5 ng/mL, semi-quantitative assay) resulted in reduced antibiotic therapy and shorter duration of hospitalization [7].
GUIDELINES
Most currently used guidelines are not able to clearly stratify patients according to their individual response to therapy, because most of the guidelines provide recommendations for a maximum duration of antibiotic therapy only in order to cover the worst-case scenario, which could result due to medico-legal reasons and non-availability of good documentable criteria for the progress of source control and treatment of systemic inflammation.
However, some recent guidelines have changed and addressed PCT-guided algorithm. For example, the updated pneumonia guideline and the sepsis guideline in Germany recommend individually adapted treatment course using PCT for diagnosis and treatment [10, 11].
In addition, the Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, published in 2012, indicate that PCT can be used for the diagnosis of sepsis and to terminate antibiotic therapy in patients who initially appeared septic, but have no subsequent evidence of infection [2].
Hence, it is expected that in future further guidelines will address the individual treatment requirements rather than a fixed treatment course with antibiotics.
SUMMARY
Daily quantitative measurement of PCT is recommended in the ICU for all critically ill patients with a suggested diagnosis of systemic inflammation, after focus removal, and immediately after onset of antibiotic therapy to monitor systemic inflammation and success of therapy.
This approach affects therapeutic and diagnostic decisions and limits the duration of antibiotic therapy, if plasma PCT levels are interpreted together with clinical signs and conventional diagnostic methods.
Further indications for PCT measurement are based on PCT induction in specific conditions, such as, bacterial sepsis, meningitis, assessment of the presence or severity of systemic inflammation, and requirement of antibiotic therapy.
In addition, PCT measurement can also be used as a tool to exclude severe systemic inflammation in patients in whom local infection or bacterial colonization is seen.
PCT can be used to guide antibiotic therapy not only in patients with lower respiratory tract infections and pneumonia, but also in patients with sepsis or severe sepsis of different source, resulting in a more rational use of antibiotics.
References+ View more
- Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006;34:1589-96.
- Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guideline for management of severe sepsis and septic shock: 2012. Crit Care Med 2013;41:580-637.
- Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C, et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised control trial. Lancet 2010;375:463-74.
- Stolz D, Smyrnios N, Eggimann P, Pargger H, Thakkar N, Siegemund M, et al. Procalcitonin for reduced antibiotic exposure in ventilator associated pneumonia: a randomised stury. Eur Respir J 2009;34:1364-75.
- Hochreiter M, Köhler T, Schweiger AM, Keck FS, Bein B, von Spiegel T, et al. Antibiotic treatment of surgical intensive care patients: procalcitonin to guide duration of therapy. Anaesthesist 2008;57:571-7.
- Schroeder S, Hochreiter M, Koehler T, Schweiger AM, Bein B, Keck FS, et al. Procalcitonin (PCT)-guided algorithm reduces length of antibiotic treatment in surgical intensive care patients with severe sepsis: results of a prospective randomized study. Langenbecks Arch Surg 2009;394:221-6.
- Qu R, JiY, Ling Y, Ye CY, Yang SM, Liu YY, et al. Procalcitonin is a good tool to guide duration of antibiotic therapy in patients with severe acute pancreatitis. A randomized prospective single-center controlled trial. Saudi Med J 2012;33:382-7.
- Briel M, Schuetz P, Mueller B, Young J, Schild U, Nusbaumer C, et al. Procalcitonin-guided antibiotic use vs a standard approach for acute respiratory tract infections in primary care. Arch Intern Med 2008;168:2000-7.
- Stolz D, Christ-Crain M, Bingisser R, Leuppi J, Miedinger D, Müller C, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest 2007;131:9-19.
- Höffken G, Lorenz J, Kern W, Welte T, Bauer T, Dalhoff K, et al. Epidemiologie, Diagnostik, antimikrobielle Therapie und Management von erwachsenen Patienten mit ambulant erworbenen unteren Atemwegsinfektionen (akute Bronchitis, akute Exazerbation einer chronischen Bronchitis, Influenza und andere respiratorische Virusinfektionen) sowie ambulant erworbener Pneumonie. Pneumonologie. 2009; 63:e1-68.
- Reinhart K, Brunkhorst FM, Bone HG, Bardutzky J, Dempfle CE, et al. Prevention, diagnosis, therapy and follow-up care of sepsis: 1st revision of S-2k guidelines of the German Sepsis Society (Deutsche Sepsis-Gesellschaft e.V. (DSG)) and the German Interdisciplinary Association of Intensive Care and Emergency Medicine (Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin (DIVI)). Ger Med Sci 2010;8:1-86.
- Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohoun C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet 1993;341:515-8.
- Linscheid P, Seboek D, Schaer JD, Zulewski H, Keller U, Müller B. Expression and secretion of procalcitonin and calcitonin gene-related peptide by adherent monocytes and macrophage-activated adipocytes. Crit Care Med 2004;32:1715-21.
- Meisner M, Müller V, Khakpour Z, Toegel E, Redl H. Induction of procalcitonin and proinflammatory cytokines in an anheptic baboon endotoxin shock model. Shock 2003;19:187-90.
- Wiedermann FJ, Kaneider N, Egger P, Tiefenthaler W, Wiedermann CJ, Lindner KH, et al. Migration of human monocytes in response to procalcitonin. Crit Care Med 2002;30:1112-7.
- Hoffmann G, Totzke G, Seibel M, Smolny M, Wiedermann FJ, Schobersberger W. In vitro modulation of inducible nitric oxide synthase gene expression and nitric oxide synthesis by procalcitonin. Crit Care Med 2001;29:112-6.
- Hoffmann G, Czechowski M, Schloesser M, Schobersberger W. Procalcitonin amplifies inducible nitric oxide synthase gene expression and nitric oxide production in vascular smooth muscle cells. Crit Care Med 2002;30:2091-5.
- Müller B, Becker KL. Procalcitonin: how a hormone became a marker and mediator of sepsis. Swiss Med Wkly 2001;131:595-602.
- Wrenger S, Kähne T, Bohuon C, Weglöhner W, Ansorge S, Reinhold D. Amino-terminal truncation of procalcitonin, a marker for systemic bacterial infections, by dipeptidyl peptidase IV (DP IV). FEBS Lett 2000;466:155-9.
- Castelli GP, Pognani C, Meisner M, Stuani A, Bellomi D, Sgarbi L. Procalcitonin and C-reactive protein during systemic inflammatory response syndrome, sepsis and organ dysfunction. Crit Care 2004;8:R234-42.
- Ugarte H, Silva E, Mercan D, De Mendonça A, Vincent JL. Procalcitonin used as a marker of infection in the intensive care unit. Crit Care Med 1999;27:498-504.
- Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret GY. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med 2006;34:1996-2003.
- Meisner M, Tschaikowsky K, Hutzler A, Schick C, Schüttler J. Postoperative plasma concentrations of procalcitonin after different types of surgery. Intensive Care Med 1998;24:680-4.
- Clec’h C, Ferriere F, Karoubi P, Fosse JP, Cupa M, Hoang P, et al. Diagnostic and prognostic value of procalcitonin in patients with septic shock. Crit Care Med 2004;32:1166-9.
- van Langevelde P, Joop K, van Loon J, Frölich M, Groeneveld PH, Westendorp RG, et al. Endotoxin, cytokines, and procalcitonin in febrile patients admitted to the hospital: identification of subjects at high risk of mortality. Clin Infect Dis 2000;31:1343-8.
- Oberhoffer M, Stonans I, Russwurm S, Stonane E, Vogelsang H, Junker U, et al. Procalcitonin expression in human peripheral blood mononuclear cells and its modulation by lipopolysaccharides and sepsis related cytokines in vitro. J Lab Clin Med 1999;134:49-55.
- Jekarl DW, Lee SY, Lee J, Park YJ, Kim Y, Park JH, et al. Procalcitonin as a diagnostic marker and IL-6 as a prognostic marker for sepsis. Diagn Microbiol Infect Dis 2013;75:342-7.
- Pfister R, Kochanek M, Leygeber T, Brun-Buisson C, Cuquemelle E, Paiva Machado MB, et al. Procalcitonin for diagnosis of bacterial pneumonia in critically illpatients during 2009 H1N1 influenza pandemic: a prospective cohort study, systematic review and individual patient data meta-analysis. Crit Care 2014;18:R44.
- Gendrel D, Raymond J, Assicot M, Moulin F, Iniguez JL, Lebon P, et al. Measurement of procalcitonin levels in children with bacterial and viral meningitis. Clin Infect Dis1997;24:1240-2.
- Moulin F, Raymond J, Lorrot M, Marc E, Coste J, Iniguez JL, et al. Procalcitonin in children admitted to hospital with community acquired pneumonia. Arch Dis Child 2001;84:332-6.
- Mathew B, Roy DD, Kumar TV. The use of procalcitonin as a marker of sepsis in children. J Clin Diagn Res 2013;7:305-7.
- Festic E, Siegel J, Stritt M, Freeman WD. The utility of serum procalcitonin in distinguishing systemic inflammatory response syndrome from infection after aneurysmal subarachnoid hemorrhage. Neurocrit Care 2014;2 [Epub ahead of print].
- Peters RP, Twisk JW, van Agtmael MA, Groeneveld AB. The role of procalcitonin in a decision tree for prediction of bloodstream infection in febrile patients. Clin Microbiol Infect 2006;12:1207-13.
- Liaudat S, Dayer E, Praz G, Bille J, Troillet N. Usefulness of procalcitonin serum level for the diagnosis of bacteremia. Eur J Clin Microbiol Infect Dis 2001;20:524-7.
- vanNieuwkoop C, Bonten TN, van´t Wout JW, Kuijper EJ, Groeneveld GH, Becker MJ, et al. Procalcitonin reflects bacteremia and bacterial load in urosepsis syndrome: a prospective observational study. Crit Care 2010;14:R206.
- Georgopoulou AP, Savva A, Giamarellos-Bourboulis EJ, Georgitsi M, Raftogiannis M, Antonakos N, et al. Early changes of procalcitonin may advise about prognosis and appropriateness of antimicrobial therapy in sepsis. J Crit Care 2011;26:331.e1-7.
- Kylänpää-Bäck ML, Takala A, Kemppainen E, Puolakkainen P, Haapiainen R, Repo H. Procalcitonin strip test in the early detection of severe acute pancreatitis. Br J Surg 2001;88:222-7.
- Rau B, Kemppainen EA, Gumbs AA, Büchler MW, Wegscheider K, Bassi C, et al. Early assessment of pancreatic infections and overall prognosis in severe acute pancreatitis by procalcitonin (PCT): a prospective international multicenter study. Ann Surg 2007;245:745-54.
- Kylänpää-Bäck ML, Takala A, Kamppainen EA, Puolakkainen PA, Leppäniemi AK, Karonen SL, et al. Procalcitonin, soluble interleukin-2 receptor, and soluble E-selectin in predicting the severity of acute pancreatitis. Crit Care Med 2001;29:63-9.
- Magrini L, Travaglino F, Marino R, Ferri E, De Berardinis B, Cardelli P, et al. Procalcitonin variations after emergency department admission are highly predictive of hospital mortality in patients with acute infectious disease. Eur Rev Med Pharmacol Sci 2013;17(S1):S113-42.
- Seligman R, Meisner M, Lisboa TC, Hertz FT, Filippin TB, Fachel JM, et al. Decreases in procalcitonin and C-reactive protein are strong predictors of survival in ventilator-associated pneumonia. Crit Care 2006;10:R125.
- Hatherill M, Tibby SM, Turner C, Ratnavel N, Murdoch IA. Procalcitonin and cytokine levels: relationship to organ failure and mortality in pediatric septic shock. Crit Care Med 2000;28:2591-4.
- Friederichs J, Hutter M, Hierholzer C, Novotny A, Friess H, Bühren V, et al. Procalcitonin ratio as a predictor of successful surgical treatment of severe necrotizing soft tissue infections. Am J Surg 2013;206:368-73.
- Meisner M, Lohs T, Huttemann E, Schmidt J, Huller M, Reinhart K. The plasma elimination rate and urinary secretion of procalcitonin in patients with normal and impaired renal function. Eur J Anaesthesiol 2001;18:79-87.
- Wojciechowicz KH, Hoffkamp HJ, van Hulst RA. Conservative treatment of acute appendicitis: an overview. Int Marit Health 2010;62:265-72.
- Ansaloni L, Catena F, Coccolini F, Ercolani G, Gazotti F, Pasqualini E, et al. Surgery versus conservative antibiotic treatment in acute appendicitiis: a systematic review and meta-analysis of randomized controlled trials. Dig Surg 2011;28:210-21.
- Chandel V, Batt SH, Bhat MY, Kawoosa NU, Yousuf A, Zargar BR. Procalcitonin as the biomarker of inflammation in diagnosis of appendicitis in pediatric patients and prevention of unneccesary appendectomies. Indian J Surg 2011;73:136-41.
- Wu JY, Chen HC, Lee SH, Chan RC, Lee CC, Chang SS. Diagnostic role of procalcitonin in patients with suspected appendicitis. Word J Surg 2012;36:1774-9.
- Kafetzis DA, Velissariou IM, Nikolaides P, Sklavos M, Maktabi M, Spyridis G, et al. Procalcitonin as a predictor of severe appendicitis in children. Eur J Clin Microbiol Infect Dis 2005;24:484-7.
- Yu CW, Juan LI, Wu MH, Shen CJ, Wu JY, Lee CC. Systematic review and meta-analysis of the diagnostic accuracy of procalcitonin, C-reactive protein and white blood cell count for suspected acute appendicitis. Br J Surg 2013;100:322-9.
- Schuetz P, Christ-Crain M, Thomann R, Falconnier C, Wolbers M, Widmer I, et al. Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections. JAMA 2009;302:1059-66.
- Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J. Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. Am J Respir Crit Care Med 2008;177:498-505.
- Gibot S. Procalcitonin in intensive care units: the PRORATA trial. Lancet 2010;375:1605-6.
- Tarnow-Mordi W and Gebski V. Procalcitonin in intensive care units: the PRORATA trial. Lancet 2010;375:1605.
- Schuetz P, Müller B, Christ-Crain M, Stolz D, Tamm M, Bouadma L, et al. Procalcitonin to initiate or discontinue antibiotiics in acute respiratory tract infections. Evid Based Child Health 2013;8:1297-371.
- Wilke MH, Grube RF, Bodmann KF. The use of standardized PCT-algorithm reduces costs in intensive care in septic patients-a DRG-based simulation model. Eur J Med Res 2011;16:543-8.
- Albrich WC, Dusemund F, Bucher B, Meyer S, Thomann R, Kühn F, et al. Effectiveness and safety of procalcitonin-guided antibiotic therapy in lower respiratory tract infections in "real life": an international, multicenter poststudy survey (ProREAL). Arch Intern Med 2012;172:715-22.
- Kook JL, Chao SR, Le J, Robinson PA. Impact of the use of procalcitonin assay in hospitalized adult patients with pneumonia at a community acute care hospital. Infect Control Hosp Epidemiol 2012;33:424-6.
- Assink-de Jong E, de Lange DW, van Oers JA, Nijsten MW, Twisk JW, Beishuizen A. Stop Antibiotics on guidance of Procalcitonin study (SAPS): a randomised prospective multicenter investigator-initiated trial to analyse whether daily measurements of procalcitonin versus a standard-of-care approach can safely shorten antibiotic duration in intensive care unit patients--caluculated sample size: 1816 patients. BMC Infect Dis 2013;13:178.
- Deliberato RO, Marra AR, Sanches PR, Martino MD, Ferreira CE, Pasternak J, et al. Clinical and economic impact of procalcitonin to shorten antimicrobial therapy in septic patients with proven bacterial infection in an intensive care setting. Diagn Microbiol Infect Dis 2013;76:266-71.
- Dusemund F, Bucher B, Meyer S, Thomann R, Kühn F, Bassetti S, et al. Influence of procalcitonin on decision to start antibiotic treatment in patients with lower respiratory tract infection: insight from the observational multicentric ProREAL surveillance. Eur J Clin Microbiol Infect Dis 2013;32:51-60.
- Annane D, Maxime V, Faller JP, Mezher C, Clec´h C, Martel P, et al. Procalcitonin levels to guide antibiotic therapy in adults with non-microbiologically proven apparent severe sepsis: a randomised controlled trial. BMJ Open 2013;3:e002186.
- Liew YX, Lee W, Cai YY, Teo J, Tang SS, Ong RW, et al. Utility and safety of procalcitonin in an antimicrobial stewardship program (ASP) in patients with malignancies. Eur J Clin Microbiol Infect Dis 2012;31:3041-6.
- Ding J, Chen Z, Feng K. Procalcitonin-guided antibiotic use in acute exacerbations of idiopathic pulmonary fibrosis. Int J Med Sci 2013;10:903-7.
- Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PR, Tamm M, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster- randomised, single-blinded intervention trial. Lancet 2004;363:600-7.
- Christ-Crain M, Stolz D, Bingisser R, Müller C, Miedinger D, Huber PR, et al. Procalcitonin-guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med 2006;174:84-93.
- Hohn A, Schroeder S, Gehrt A, Bernhardt K, Bein B, Wegscheider K, et al. Procalcitonin-guided algorithm to reduce length of antibiotic therapy in patients with severe sepsis and septic shock. BMC Infect Dis 2013;13:158.
- Meisner M, Hutzler A, Tschaikowsky K, Harig F, von der Emde J. Postoperative plasma concentration of procalcitonin and C-reactive protein in patients undergoing cardiac and thoracic surgery with and without cardiopulmonary bypass. Cardiovasc Eng 1998;3:174-8.
- Syvänen J, Peltola V, Pajulo O, Ruuskanen O, Mertsola J, Helenius I. Normal behaviour of plasma procalcitonin in adolescents undergoing surgery for scoliosis. Scand J Surg 2014;103:60-5.
- Wanner GA, Keel M, Steckholzer U, Beier W, Stocker R, Ertel W. Relationship between procalcitonin plasma levels and severity of injury, sepsis, organ failure, and mortality in injured patients. Crit Care Med 2000;28:950-7.
- Meisner M, Heide A, Schmidt J. Correlation of procalcitonin and C-reactive protein to inflammation, complications, and outcome during the intensive care unit course of multiple-trauma patients. Crit Care 2006:10:R1.
- vonHeimburg D, Stieghorst W, Khorram-Sefat R, Pallua N. Procalcitonin -- a sepsis parameter in severe burn injuries. Burns 1998;24:745-50.
- Lavrentieva A, Kontakiotis T, Lazaridis L, Tsotolis N, Koumis J, Kyriazis G, et al. Inflammatory markers in patients with severe burn injury. What is the best indicator of sepsis? Burns 2007;33:189-94.
- Ulrich D, Noah EM, Pallua N. Plasma endotoxin, procalcitonin, C-reaktives protein, andorgan functions in patients with major burns. Handchir Mikrochir Plast Chir 2001;33:262-6.
- Carsin H, Assicot M, Feger F, Roy O, Pennacino I, Le Bever H, et al. Evolution and significance of circulating procalcitonin levels compared with IL-6, TNFα and endotoxin levels early after thermal injury. Burns 1997;23:218-24.
- de Werra I, Jaccard C, Corradin SB, Chioléro R, Yersin B, Gallati H, et al. Cytokines, nitrite/nitrate, soluble tumor necrosis factor receptors, and procalcitonin concentrations: Comparisons in patients with septic shock, cardiogenic shock, and bacterial pneumonia. Crit Care Med 1997;25:607-13.
- Brunkhorst FM, Forycki ZF, Wagner J. Procalcitonin-immunoreactivity in patients with cardiogenic shock- does bacterial inflammation influence the prognosis? Eur Heart J 1996;17(S2):S67-72.
- Geppert A, Steiner A, Delle-Karth G, Heinz G, Huber K. Usefulness of procalcitonin for diagnosing complicating sepsis in patients with cardiogenic shock. Intensive Care Med 2003;29:1384-9.
- Nylén ES, Al Arifi A, Becker KL, Snider RH Jr, Alzeer A. Effect of classic heatstroke on serum procalcitonin. Crit Care Med 1997;25:1362-5.
- Hausfater P, Hurtado M, Pease S, Juillien G, Lvovschi VE, Salehabadi S, et al. Is procalcitonin a marker of criticall illness in heatstroke? Intensive Care Med 2008;34:1377-83.
- Sabat R, Höflich C, Döcke WD, Oppert M, Kern F, Windrich B, et al. Massive elevation of procalcitonin plasma levels in the absence of infection in kidney transplant patients treated with pan-T-cell antibodies. Intensive Care Med 2001;27:987-91.
- Abramowicz D, Schandene L, Goldmann M, Crusiaux A, Vareerstraeten P, De Pauw L, et al. Release of tumor necrosis factor, interleukin-2, and gamma-interferon in serum after injection of OKT3 monoclonal antibody in kidney transplant recipients. Transplantation 1989;47:606-8.
- Rau B, Steinbach G, Baumgart K, Gansauge F, Grünert A, Beger HG. The clinical value of procalcitonin in the prediction of infected necrosis in acute pancreatitis. Intensive Care Med 2000;26(S2):S159-64.
- Scirè CA, Cavagna L, Perotti C, Bruschi E, Caporali R, Montecucco C. Diagnostic value of procalcitonin measurement in febrile patients with systemic autoimmune diseases. ClinExpRheumatol 2006;24:123-8.
- Korczowski B. Serum procalcitonin concentration in children with liver disease. Pediatr Infect Dis J 2006;25:268-9.
- Delèvaux I, André M, Colombier M, Albuisson E, Meylheuc F, Bègue RJ, et al. Can procalcitonin measurement help in differentiating between bacterial infection and other kinds of inflammatory processes ? Ann Rheum Dis 2003;62:337-40.
- Scirè CA, Caporali R, Perotti C, Montecucco C. Plasma procalcitonin in rheumatic diseases. Reumatismo 2003;55:113-8.
- Kádár J and Petrovicz E. Adult-onset Still´s disease. Best Pract Res Clin Rheumatol 2004;18:663-76.
- Moosig F, Csernok E, Reinhold-Keller E, Schmitt W, Gross WL. Elevated procalcitonin levels in active Wegener’s granulomatosis. J Rheumatol 1998;25:1531-3.
- Eberhard OK, Haubitz M, Brunkhorst FM, Kliem V, Koch KM, Brunkhorst R. Usefulness of procalcitonin for differentiation between activity of systemic autoimmune disease (systemic lupus erythematosus/systemic antineutrophil cytoplasmatic antibody-associated vasculitis) and invasive bacterial infection. Arthritis Rheum 1997;40:1250-6.
- Dahaba AA, Rehak PH, List WF. Procalcitonin and C-reactive protein plasma concentrations in nonseptic uremic patients undergoing hemodialysis. Intensive Care Med 2003;29:579-83.
- Steinbach G, Bölke E, Grünert A, Störck M, Orth K. Procalcitonin in patients with acute and chronic renal insufficiency. Wien Klin Wochenschr 2004;116:849-53.
- Meisner M, Hüttemann E, Lohs T, Kasakov L, Reinhart K. Plasma concentrations and clearance of procalcitonin during continuous veno-venous hemofiltration in septic patients. Shock 2001;15:171-5.
- Schmidt M, Burchardi C, Sitter T, Held E, Schiffl H. Procalcitonin in patients undergoing chronic hemodialysis. Nephron 2000;84:187-8.
- Elefsiniotis IS, Skounakis M, Vezali M, Pantazis KD, Petrocheilou A, Pirounaki M, et al. Clinical significance of serum procalcitonin levels in patients with acute or chronic liver disease. Eur J Gastroenterol Hepatol 2006;18:525-30.
- Attar BM, Moore CM, George M, Ion-Nedelcu N, Turbay R, Zachariah A, et al. Procalcitonin, and cytokines document a dynamic inflammatory state in non-infected cirrhotic patients with ascites. World J Gastroenterol 2014;20:2374-82.
- Fries M, Kunz D, Gressner AM, Roissant R, Kuhlen R. Procalcitonin serum levels after ouf-of-hospital cardiac arrest. Resuscitation 2003;59:105-9.
- Oppert M, Reinicke A, Müller C, Barckow D, Frei U, Eckard KU. Elevations in procalcitonin but not C-reactive protein are associated with pneumonia after cardiopulmonary resuscitation. Resuscitation 2002;53:167-70.
- Chiesa C, Panero A, Rossi N, Stegagno M, De Giusti M, Osborn JF, et al. Reliability of procalcitonin concentrations for the diagnosis of sepsis in critically ill neonates. Clin Infect Dis 1998;26:664-72.
- Turner D, Hammerman C, Rudensky B, Schlesinger Y, Goia C, Schimmel MS. Procalcitonin in preterm infants during the first few days of life: introducing an age related nomogram. Arch Dis Child Fetal Neonatal Ed 2006;91:F283-6.
- Stocker M, Fontana M, El Helou S, Wegscheider K, Berger TM. Use of procalcitonin-guided decision-making to shorten antibiotic therapy in suspected neonatal early-onset sepsis: prospective randomized intervention trial. Neonatology 2010;97:165-74.
- Lencot S, Cabaret B, Sauvage G, Laurans C, Launay E, Orsonneau JL, et al. A new procalcitonin cord-based algorithm in early-onset neonatal infection: for a change of paradigm. Eur J Clin Microbiol Infect Dis 2014 [Epub ahead of print].
- Jimeno A, García-Velasco A, del Val O, González-Billalabeitia E, Hernando S, Hernández R, et al. Assessment of procalcitonin as a diagnostic and prognostic marker in patients with solid tumors and febrile neutropenia. Cancer 2004;100:2462-9.
- Bihan H, Becker KL, Snider RH, Nylen E, Vittaz L, Lauret C, et al. Calcitonin precursor levels in human medullary thyroid carcinoma. Thyroid 2003;13:819-22.
- Morgenthaler NG, Struck J, Fischer-Schulz C, Seidel-Mueller E, Beier W, Bergmann A. Detection of Procalcitonin (PCT) in healthy controls and patients with local infection by a sensitive ILMA. Clin Lab 2002; 48: 263-270.
References
- Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006;34:1589-96.
- Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guideline for management of severe sepsis and septic shock: 2012. Crit Care Med 2013;41:580-637.
- Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C, et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised control trial. Lancet 2010;375:463-74.
- Stolz D, Smyrnios N, Eggimann P, Pargger H, Thakkar N, Siegemund M, et al. Procalcitonin for reduced antibiotic exposure in ventilator associated pneumonia: a randomised stury. Eur Respir J 2009;34:1364-75.
- Hochreiter M, Köhler T, Schweiger AM, Keck FS, Bein B, von Spiegel T, et al. Antibiotic treatment of surgical intensive care patients: procalcitonin to guide duration of therapy. Anaesthesist 2008;57:571-7.
- Schroeder S, Hochreiter M, Koehler T, Schweiger AM, Bein B, Keck FS, et al. Procalcitonin (PCT)-guided algorithm reduces length of antibiotic treatment in surgical intensive care patients with severe sepsis: results of a prospective randomized study. Langenbecks Arch Surg 2009;394:221-6.
- Qu R, JiY, Ling Y, Ye CY, Yang SM, Liu YY, et al. Procalcitonin is a good tool to guide duration of antibiotic therapy in patients with severe acute pancreatitis. A randomized prospective single-center controlled trial. Saudi Med J 2012;33:382-7.
- Briel M, Schuetz P, Mueller B, Young J, Schild U, Nusbaumer C, et al. Procalcitonin-guided antibiotic use vs a standard approach for acute respiratory tract infections in primary care. Arch Intern Med 2008;168:2000-7.
- Stolz D, Christ-Crain M, Bingisser R, Leuppi J, Miedinger D, Müller C, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest 2007;131:9-19.
- Höffken G, Lorenz J, Kern W, Welte T, Bauer T, Dalhoff K, et al. Epidemiologie, Diagnostik, antimikrobielle Therapie und Management von erwachsenen Patienten mit ambulant erworbenen unteren Atemwegsinfektionen (akute Bronchitis, akute Exazerbation einer chronischen Bronchitis, Influenza und andere respiratorische Virusinfektionen) sowie ambulant erworbener Pneumonie. Pneumonologie. 2009; 63:e1-68.
- Reinhart K, Brunkhorst FM, Bone HG, Bardutzky J, Dempfle CE, et al. Prevention, diagnosis, therapy and follow-up care of sepsis: 1st revision of S-2k guidelines of the German Sepsis Society (Deutsche Sepsis-Gesellschaft e.V. (DSG)) and the German Interdisciplinary Association of Intensive Care and Emergency Medicine (Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin (DIVI)). Ger Med Sci 2010;8:1-86.
- Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohoun C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet 1993;341:515-8.
- Linscheid P, Seboek D, Schaer JD, Zulewski H, Keller U, Müller B. Expression and secretion of procalcitonin and calcitonin gene-related peptide by adherent monocytes and macrophage-activated adipocytes. Crit Care Med 2004;32:1715-21.
- Meisner M, Müller V, Khakpour Z, Toegel E, Redl H. Induction of procalcitonin and proinflammatory cytokines in an anheptic baboon endotoxin shock model. Shock 2003;19:187-90.
- Wiedermann FJ, Kaneider N, Egger P, Tiefenthaler W, Wiedermann CJ, Lindner KH, et al. Migration of human monocytes in response to procalcitonin. Crit Care Med 2002;30:1112-7.
- Hoffmann G, Totzke G, Seibel M, Smolny M, Wiedermann FJ, Schobersberger W. In vitro modulation of inducible nitric oxide synthase gene expression and nitric oxide synthesis by procalcitonin. Crit Care Med 2001;29:112-6.
- Hoffmann G, Czechowski M, Schloesser M, Schobersberger W. Procalcitonin amplifies inducible nitric oxide synthase gene expression and nitric oxide production in vascular smooth muscle cells. Crit Care Med 2002;30:2091-5.
- Müller B, Becker KL. Procalcitonin: how a hormone became a marker and mediator of sepsis. Swiss Med Wkly 2001;131:595-602.
- Wrenger S, Kähne T, Bohuon C, Weglöhner W, Ansorge S, Reinhold D. Amino-terminal truncation of procalcitonin, a marker for systemic bacterial infections, by dipeptidyl peptidase IV (DP IV). FEBS Lett 2000;466:155-9.
- Castelli GP, Pognani C, Meisner M, Stuani A, Bellomi D, Sgarbi L. Procalcitonin and C-reactive protein during systemic inflammatory response syndrome, sepsis and organ dysfunction. Crit Care 2004;8:R234-42.
- Ugarte H, Silva E, Mercan D, De Mendonça A, Vincent JL. Procalcitonin used as a marker of infection in the intensive care unit. Crit Care Med 1999;27:498-504.
- Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret GY. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med 2006;34:1996-2003.
- Meisner M, Tschaikowsky K, Hutzler A, Schick C, Schüttler J. Postoperative plasma concentrations of procalcitonin after different types of surgery. Intensive Care Med 1998;24:680-4.
- Clec’h C, Ferriere F, Karoubi P, Fosse JP, Cupa M, Hoang P, et al. Diagnostic and prognostic value of procalcitonin in patients with septic shock. Crit Care Med 2004;32:1166-9.
- van Langevelde P, Joop K, van Loon J, Frölich M, Groeneveld PH, Westendorp RG, et al. Endotoxin, cytokines, and procalcitonin in febrile patients admitted to the hospital: identification of subjects at high risk of mortality. Clin Infect Dis 2000;31:1343-8.
- Oberhoffer M, Stonans I, Russwurm S, Stonane E, Vogelsang H, Junker U, et al. Procalcitonin expression in human peripheral blood mononuclear cells and its modulation by lipopolysaccharides and sepsis related cytokines in vitro. J Lab Clin Med 1999;134:49-55.
- Jekarl DW, Lee SY, Lee J, Park YJ, Kim Y, Park JH, et al. Procalcitonin as a diagnostic marker and IL-6 as a prognostic marker for sepsis. Diagn Microbiol Infect Dis 2013;75:342-7.
- Pfister R, Kochanek M, Leygeber T, Brun-Buisson C, Cuquemelle E, Paiva Machado MB, et al. Procalcitonin for diagnosis of bacterial pneumonia in critically illpatients during 2009 H1N1 influenza pandemic: a prospective cohort study, systematic review and individual patient data meta-analysis. Crit Care 2014;18:R44.
- Gendrel D, Raymond J, Assicot M, Moulin F, Iniguez JL, Lebon P, et al. Measurement of procalcitonin levels in children with bacterial and viral meningitis. Clin Infect Dis1997;24:1240-2.
- Moulin F, Raymond J, Lorrot M, Marc E, Coste J, Iniguez JL, et al. Procalcitonin in children admitted to hospital with community acquired pneumonia. Arch Dis Child 2001;84:332-6.
- Mathew B, Roy DD, Kumar TV. The use of procalcitonin as a marker of sepsis in children. J Clin Diagn Res 2013;7:305-7.
- Festic E, Siegel J, Stritt M, Freeman WD. The utility of serum procalcitonin in distinguishing systemic inflammatory response syndrome from infection after aneurysmal subarachnoid hemorrhage. Neurocrit Care 2014;2 [Epub ahead of print].
- Peters RP, Twisk JW, van Agtmael MA, Groeneveld AB. The role of procalcitonin in a decision tree for prediction of bloodstream infection in febrile patients. Clin Microbiol Infect 2006;12:1207-13.
- Liaudat S, Dayer E, Praz G, Bille J, Troillet N. Usefulness of procalcitonin serum level for the diagnosis of bacteremia. Eur J Clin Microbiol Infect Dis 2001;20:524-7.
- vanNieuwkoop C, Bonten TN, van´t Wout JW, Kuijper EJ, Groeneveld GH, Becker MJ, et al. Procalcitonin reflects bacteremia and bacterial load in urosepsis syndrome: a prospective observational study. Crit Care 2010;14:R206.
- Georgopoulou AP, Savva A, Giamarellos-Bourboulis EJ, Georgitsi M, Raftogiannis M, Antonakos N, et al. Early changes of procalcitonin may advise about prognosis and appropriateness of antimicrobial therapy in sepsis. J Crit Care 2011;26:331.e1-7.
- Kylänpää-Bäck ML, Takala A, Kemppainen E, Puolakkainen P, Haapiainen R, Repo H. Procalcitonin strip test in the early detection of severe acute pancreatitis. Br J Surg 2001;88:222-7.
- Rau B, Kemppainen EA, Gumbs AA, Büchler MW, Wegscheider K, Bassi C, et al. Early assessment of pancreatic infections and overall prognosis in severe acute pancreatitis by procalcitonin (PCT): a prospective international multicenter study. Ann Surg 2007;245:745-54.
- Kylänpää-Bäck ML, Takala A, Kamppainen EA, Puolakkainen PA, Leppäniemi AK, Karonen SL, et al. Procalcitonin, soluble interleukin-2 receptor, and soluble E-selectin in predicting the severity of acute pancreatitis. Crit Care Med 2001;29:63-9.
- Magrini L, Travaglino F, Marino R, Ferri E, De Berardinis B, Cardelli P, et al. Procalcitonin variations after emergency department admission are highly predictive of hospital mortality in patients with acute infectious disease. Eur Rev Med Pharmacol Sci 2013;17(S1):S113-42.
- Seligman R, Meisner M, Lisboa TC, Hertz FT, Filippin TB, Fachel JM, et al. Decreases in procalcitonin and C-reactive protein are strong predictors of survival in ventilator-associated pneumonia. Crit Care 2006;10:R125.
- Hatherill M, Tibby SM, Turner C, Ratnavel N, Murdoch IA. Procalcitonin and cytokine levels: relationship to organ failure and mortality in pediatric septic shock. Crit Care Med 2000;28:2591-4.
- Friederichs J, Hutter M, Hierholzer C, Novotny A, Friess H, Bühren V, et al. Procalcitonin ratio as a predictor of successful surgical treatment of severe necrotizing soft tissue infections. Am J Surg 2013;206:368-73.
- Meisner M, Lohs T, Huttemann E, Schmidt J, Huller M, Reinhart K. The plasma elimination rate and urinary secretion of procalcitonin in patients with normal and impaired renal function. Eur J Anaesthesiol 2001;18:79-87.
- Wojciechowicz KH, Hoffkamp HJ, van Hulst RA. Conservative treatment of acute appendicitis: an overview. Int Marit Health 2010;62:265-72.
- Ansaloni L, Catena F, Coccolini F, Ercolani G, Gazotti F, Pasqualini E, et al. Surgery versus conservative antibiotic treatment in acute appendicitiis: a systematic review and meta-analysis of randomized controlled trials. Dig Surg 2011;28:210-21.
- Chandel V, Batt SH, Bhat MY, Kawoosa NU, Yousuf A, Zargar BR. Procalcitonin as the biomarker of inflammation in diagnosis of appendicitis in pediatric patients and prevention of unneccesary appendectomies. Indian J Surg 2011;73:136-41.
- Wu JY, Chen HC, Lee SH, Chan RC, Lee CC, Chang SS. Diagnostic role of procalcitonin in patients with suspected appendicitis. Word J Surg 2012;36:1774-9.
- Kafetzis DA, Velissariou IM, Nikolaides P, Sklavos M, Maktabi M, Spyridis G, et al. Procalcitonin as a predictor of severe appendicitis in children. Eur J Clin Microbiol Infect Dis 2005;24:484-7.
- Yu CW, Juan LI, Wu MH, Shen CJ, Wu JY, Lee CC. Systematic review and meta-analysis of the diagnostic accuracy of procalcitonin, C-reactive protein and white blood cell count for suspected acute appendicitis. Br J Surg 2013;100:322-9.
- Schuetz P, Christ-Crain M, Thomann R, Falconnier C, Wolbers M, Widmer I, et al. Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections. JAMA 2009;302:1059-66.
- Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J. Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. Am J Respir Crit Care Med 2008;177:498-505.
- Gibot S. Procalcitonin in intensive care units: the PRORATA trial. Lancet 2010;375:1605-6.
- Tarnow-Mordi W and Gebski V. Procalcitonin in intensive care units: the PRORATA trial. Lancet 2010;375:1605.
- Schuetz P, Müller B, Christ-Crain M, Stolz D, Tamm M, Bouadma L, et al. Procalcitonin to initiate or discontinue antibiotiics in acute respiratory tract infections. Evid Based Child Health 2013;8:1297-371.
- Wilke MH, Grube RF, Bodmann KF. The use of standardized PCT-algorithm reduces costs in intensive care in septic patients-a DRG-based simulation model. Eur J Med Res 2011;16:543-8.
- Albrich WC, Dusemund F, Bucher B, Meyer S, Thomann R, Kühn F, et al. Effectiveness and safety of procalcitonin-guided antibiotic therapy in lower respiratory tract infections in "real life": an international, multicenter poststudy survey (ProREAL). Arch Intern Med 2012;172:715-22.
- Kook JL, Chao SR, Le J, Robinson PA. Impact of the use of procalcitonin assay in hospitalized adult patients with pneumonia at a community acute care hospital. Infect Control Hosp Epidemiol 2012;33:424-6.
- Assink-de Jong E, de Lange DW, van Oers JA, Nijsten MW, Twisk JW, Beishuizen A. Stop Antibiotics on guidance of Procalcitonin study (SAPS): a randomised prospective multicenter investigator-initiated trial to analyse whether daily measurements of procalcitonin versus a standard-of-care approach can safely shorten antibiotic duration in intensive care unit patients--caluculated sample size: 1816 patients. BMC Infect Dis 2013;13:178.
- Deliberato RO, Marra AR, Sanches PR, Martino MD, Ferreira CE, Pasternak J, et al. Clinical and economic impact of procalcitonin to shorten antimicrobial therapy in septic patients with proven bacterial infection in an intensive care setting. Diagn Microbiol Infect Dis 2013;76:266-71.
- Dusemund F, Bucher B, Meyer S, Thomann R, Kühn F, Bassetti S, et al. Influence of procalcitonin on decision to start antibiotic treatment in patients with lower respiratory tract infection: insight from the observational multicentric ProREAL surveillance. Eur J Clin Microbiol Infect Dis 2013;32:51-60.
- Annane D, Maxime V, Faller JP, Mezher C, Clec´h C, Martel P, et al. Procalcitonin levels to guide antibiotic therapy in adults with non-microbiologically proven apparent severe sepsis: a randomised controlled trial. BMJ Open 2013;3:e002186.
- Liew YX, Lee W, Cai YY, Teo J, Tang SS, Ong RW, et al. Utility and safety of procalcitonin in an antimicrobial stewardship program (ASP) in patients with malignancies. Eur J Clin Microbiol Infect Dis 2012;31:3041-6.
- Ding J, Chen Z, Feng K. Procalcitonin-guided antibiotic use in acute exacerbations of idiopathic pulmonary fibrosis. Int J Med Sci 2013;10:903-7.
- Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PR, Tamm M, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster- randomised, single-blinded intervention trial. Lancet 2004;363:600-7.
- Christ-Crain M, Stolz D, Bingisser R, Müller C, Miedinger D, Huber PR, et al. Procalcitonin-guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med 2006;174:84-93.
- Hohn A, Schroeder S, Gehrt A, Bernhardt K, Bein B, Wegscheider K, et al. Procalcitonin-guided algorithm to reduce length of antibiotic therapy in patients with severe sepsis and septic shock. BMC Infect Dis 2013;13:158.
- Meisner M, Hutzler A, Tschaikowsky K, Harig F, von der Emde J. Postoperative plasma concentration of procalcitonin and C-reactive protein in patients undergoing cardiac and thoracic surgery with and without cardiopulmonary bypass. Cardiovasc Eng 1998;3:174-8.
- Syvänen J, Peltola V, Pajulo O, Ruuskanen O, Mertsola J, Helenius I. Normal behaviour of plasma procalcitonin in adolescents undergoing surgery for scoliosis. Scand J Surg 2014;103:60-5.
- Wanner GA, Keel M, Steckholzer U, Beier W, Stocker R, Ertel W. Relationship between procalcitonin plasma levels and severity of injury, sepsis, organ failure, and mortality in injured patients. Crit Care Med 2000;28:950-7.
- Meisner M, Heide A, Schmidt J. Correlation of procalcitonin and C-reactive protein to inflammation, complications, and outcome during the intensive care unit course of multiple-trauma patients. Crit Care 2006:10:R1.
- vonHeimburg D, Stieghorst W, Khorram-Sefat R, Pallua N. Procalcitonin -- a sepsis parameter in severe burn injuries. Burns 1998;24:745-50.
- Lavrentieva A, Kontakiotis T, Lazaridis L, Tsotolis N, Koumis J, Kyriazis G, et al. Inflammatory markers in patients with severe burn injury. What is the best indicator of sepsis? Burns 2007;33:189-94.
- Ulrich D, Noah EM, Pallua N. Plasma endotoxin, procalcitonin, C-reaktives protein, andorgan functions in patients with major burns. Handchir Mikrochir Plast Chir 2001;33:262-6.
- Carsin H, Assicot M, Feger F, Roy O, Pennacino I, Le Bever H, et al. Evolution and significance of circulating procalcitonin levels compared with IL-6, TNFα and endotoxin levels early after thermal injury. Burns 1997;23:218-24.
- de Werra I, Jaccard C, Corradin SB, Chioléro R, Yersin B, Gallati H, et al. Cytokines, nitrite/nitrate, soluble tumor necrosis factor receptors, and procalcitonin concentrations: Comparisons in patients with septic shock, cardiogenic shock, and bacterial pneumonia. Crit Care Med 1997;25:607-13.
- Brunkhorst FM, Forycki ZF, Wagner J. Procalcitonin-immunoreactivity in patients with cardiogenic shock- does bacterial inflammation influence the prognosis? Eur Heart J 1996;17(S2):S67-72.
- Geppert A, Steiner A, Delle-Karth G, Heinz G, Huber K. Usefulness of procalcitonin for diagnosing complicating sepsis in patients with cardiogenic shock. Intensive Care Med 2003;29:1384-9.
- Nylén ES, Al Arifi A, Becker KL, Snider RH Jr, Alzeer A. Effect of classic heatstroke on serum procalcitonin. Crit Care Med 1997;25:1362-5.
- Hausfater P, Hurtado M, Pease S, Juillien G, Lvovschi VE, Salehabadi S, et al. Is procalcitonin a marker of criticall illness in heatstroke? Intensive Care Med 2008;34:1377-83.
- Sabat R, Höflich C, Döcke WD, Oppert M, Kern F, Windrich B, et al. Massive elevation of procalcitonin plasma levels in the absence of infection in kidney transplant patients treated with pan-T-cell antibodies. Intensive Care Med 2001;27:987-91.
- Abramowicz D, Schandene L, Goldmann M, Crusiaux A, Vareerstraeten P, De Pauw L, et al. Release of tumor necrosis factor, interleukin-2, and gamma-interferon in serum after injection of OKT3 monoclonal antibody in kidney transplant recipients. Transplantation 1989;47:606-8.
- Rau B, Steinbach G, Baumgart K, Gansauge F, Grünert A, Beger HG. The clinical value of procalcitonin in the prediction of infected necrosis in acute pancreatitis. Intensive Care Med 2000;26(S2):S159-64.
- Scirè CA, Cavagna L, Perotti C, Bruschi E, Caporali R, Montecucco C. Diagnostic value of procalcitonin measurement in febrile patients with systemic autoimmune diseases. ClinExpRheumatol 2006;24:123-8.
- Korczowski B. Serum procalcitonin concentration in children with liver disease. Pediatr Infect Dis J 2006;25:268-9.
- Delèvaux I, André M, Colombier M, Albuisson E, Meylheuc F, Bègue RJ, et al. Can procalcitonin measurement help in differentiating between bacterial infection and other kinds of inflammatory processes ? Ann Rheum Dis 2003;62:337-40.
- Scirè CA, Caporali R, Perotti C, Montecucco C. Plasma procalcitonin in rheumatic diseases. Reumatismo 2003;55:113-8.
- Kádár J and Petrovicz E. Adult-onset Still´s disease. Best Pract Res Clin Rheumatol 2004;18:663-76.
- Moosig F, Csernok E, Reinhold-Keller E, Schmitt W, Gross WL. Elevated procalcitonin levels in active Wegener’s granulomatosis. J Rheumatol 1998;25:1531-3.
- Eberhard OK, Haubitz M, Brunkhorst FM, Kliem V, Koch KM, Brunkhorst R. Usefulness of procalcitonin for differentiation between activity of systemic autoimmune disease (systemic lupus erythematosus/systemic antineutrophil cytoplasmatic antibody-associated vasculitis) and invasive bacterial infection. Arthritis Rheum 1997;40:1250-6.
- Dahaba AA, Rehak PH, List WF. Procalcitonin and C-reactive protein plasma concentrations in nonseptic uremic patients undergoing hemodialysis. Intensive Care Med 2003;29:579-83.
- Steinbach G, Bölke E, Grünert A, Störck M, Orth K. Procalcitonin in patients with acute and chronic renal insufficiency. Wien Klin Wochenschr 2004;116:849-53.
- Meisner M, Hüttemann E, Lohs T, Kasakov L, Reinhart K. Plasma concentrations and clearance of procalcitonin during continuous veno-venous hemofiltration in septic patients. Shock 2001;15:171-5.
- Schmidt M, Burchardi C, Sitter T, Held E, Schiffl H. Procalcitonin in patients undergoing chronic hemodialysis. Nephron 2000;84:187-8.
- Elefsiniotis IS, Skounakis M, Vezali M, Pantazis KD, Petrocheilou A, Pirounaki M, et al. Clinical significance of serum procalcitonin levels in patients with acute or chronic liver disease. Eur J Gastroenterol Hepatol 2006;18:525-30.
- Attar BM, Moore CM, George M, Ion-Nedelcu N, Turbay R, Zachariah A, et al. Procalcitonin, and cytokines document a dynamic inflammatory state in non-infected cirrhotic patients with ascites. World J Gastroenterol 2014;20:2374-82.
- Fries M, Kunz D, Gressner AM, Roissant R, Kuhlen R. Procalcitonin serum levels after ouf-of-hospital cardiac arrest. Resuscitation 2003;59:105-9.
- Oppert M, Reinicke A, Müller C, Barckow D, Frei U, Eckard KU. Elevations in procalcitonin but not C-reactive protein are associated with pneumonia after cardiopulmonary resuscitation. Resuscitation 2002;53:167-70.
- Chiesa C, Panero A, Rossi N, Stegagno M, De Giusti M, Osborn JF, et al. Reliability of procalcitonin concentrations for the diagnosis of sepsis in critically ill neonates. Clin Infect Dis 1998;26:664-72.
- Turner D, Hammerman C, Rudensky B, Schlesinger Y, Goia C, Schimmel MS. Procalcitonin in preterm infants during the first few days of life: introducing an age related nomogram. Arch Dis Child Fetal Neonatal Ed 2006;91:F283-6.
- Stocker M, Fontana M, El Helou S, Wegscheider K, Berger TM. Use of procalcitonin-guided decision-making to shorten antibiotic therapy in suspected neonatal early-onset sepsis: prospective randomized intervention trial. Neonatology 2010;97:165-74.
- Lencot S, Cabaret B, Sauvage G, Laurans C, Launay E, Orsonneau JL, et al. A new procalcitonin cord-based algorithm in early-onset neonatal infection: for a change of paradigm. Eur J Clin Microbiol Infect Dis 2014 [Epub ahead of print].
- Jimeno A, García-Velasco A, del Val O, González-Billalabeitia E, Hernando S, Hernández R, et al. Assessment of procalcitonin as a diagnostic and prognostic marker in patients with solid tumors and febrile neutropenia. Cancer 2004;100:2462-9.
- Bihan H, Becker KL, Snider RH, Nylen E, Vittaz L, Lauret C, et al. Calcitonin precursor levels in human medullary thyroid carcinoma. Thyroid 2003;13:819-22.
- Morgenthaler NG, Struck J, Fischer-Schulz C, Seidel-Mueller E, Beier W, Bergmann A. Detection of Procalcitonin (PCT) in healthy controls and patients with local infection by a sensitive ILMA. Clin Lab 2002; 48: 263-270.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info.
Acute care testing handbook
Get the acute care testing handbook
Your practical guide to critical parameters in acute care testing.
Download nowScientific webinars
Check out the list of webinars
Radiometer and acutecaretesting.org present free educational webinars on topics surrounding acute care testing presented by international experts.
Go to webinars








