Printed from acutecaretesting.org
April 2014
Natriuretic peptide testing for heart failure diagnosis, inpatient management and outpatient cardiac care
INTRODUCTIONA common reason for patients to visit the emergency room is acute shortness of breath (acute dyspnea). A serious cause of acute shortness of breath can be heart failure. Accurate diagnosis of heart failure is known to be a significant challenge for healthcare professionals in emergency departments (EDs) [1]. |
|
Complex cases, combined with limitations on time, specialist staff and investigations create uncertainty around admissions and difficulties when communicating with intensive care units (ICUs) and other departments [1]. In a recent US study, 30-day readmission rates for heart failure were high, at 25 % which could be related to these uncertainties [2].
Lengthy patient evaluation and turnaround times coupled with late or incorrect diagnosis and treatment result in higher morbidity and mortality, as well as increasing treatment costs [1,3].
This paper provides a practical overview of the potential for natriuretic peptide (NP) testing to help streamline care pathways and improve outcomes, in both the acute and chronic cardiac care settings.
NATRIURETIC PEPTIDE SYNTHESIS, RELEASE AND DETECTION
The brain natriuretic peptide (BNP) gene is activated in cardiomyocytes when myocardial wall stress is increased by an overload of volume or pressure [4]. The resulting precursor peptide (proBNP108) is cleaved into two parts: active BNP, and inactive N-terminal (NT)-proBNP, which are released into the circulation (Fig. 1) [5].
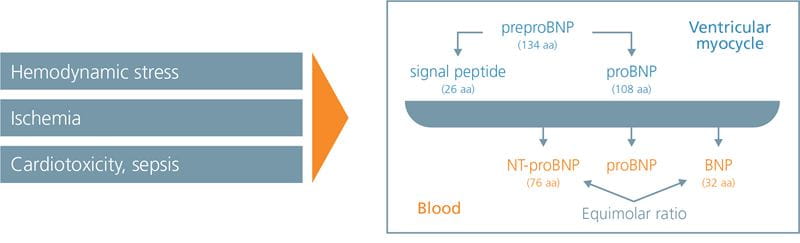
FIG. 1: BNP and NT-proBNP are secreted from cardiomyocytes at the same time
Adapted from Martinez-Rumayor A, Richards AM, Burnett JC, Januzzi JL. Biology of the Natriuretic Peptides. Am J Cardiol
2008;101[Suppl]: 3A–8A).
ProBNP108, as well as various degradation products of BNP, can also be found in the bloodstream [4]. In cases of heart failure, a large increase in the usually low BNP levels occurs, leading to positive downstream effects, including vasorelaxation and natriuresis [4].
Both BNP and NT-proBNP can be detected in the circulation. Whilst increased levels of these biomarkers are not exclusive to incidences of heart failure, studies have shown that they can be sensitive and specific diagnostic biomarkers for heart failure when used as an adjunct to clinical judgment [6,7]. The 2012 European Society of Cardiology (ESC) and 2013 American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines name BNP and NT-proBNP as suitable biomarkers, along with a medical history, physical examination and ECG, for the diagnosis, prognosis and management of patients with acute and non-acute onset heart failure [8,9].
USING NATRIURETIC PEPTIDES TO INCREASE ACCURACY OF DECISION-MAKING IN THE EMERGENCY SETTING
Heart failure is defined by the presence of typical symptoms such as dyspnea, fatigue and/or fluid retention due to cardiac dysfunction. These typical, yet non-specific symptoms can make heart failure difficult to diagnose [8]. Inaccurate emergency diagnosis of elderly patients with acute respiratory failure was shown to be as high as 20 % by the French EPIDASA Study Group [10]. These missed diagnoses were associated with highly significant increases in mortality, and highlighted the need for diagnostic tools with high specificity and sensitivity that can be accessed quickly in a busy ED environment [10].
The potential for NPs to augment clinical judgment and standard diagnostic tools has been identified in US and European studies. In the US Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT), physicians were blinded to BNP levels when making admission decisions, and on analysis, BNP levels were in fact higher in those patients who were discharged [11].
In fact, BNP levels were more than twice as high (2,096 vs. 764 pg/mL) in patients who were deceased at 30 days vs. those who were alive [10]. This pattern was maintained at 90 days, indicating that BNP would indeed have been useful when deciding whether a patient should have been admitted [11].
By helping to confirm or rule out a diagnosis of heart failure, NPs can help inform and expedite treatment decisions. Faster BNP measurement was associated with more expedient initiation of diuretic therapy, with a modest improvement in mortality in an analysis of US Acute Decompensated Heart Failure National Registry (ADHERE) study data [12].
Looking at NP testing as part of the overall care pathway, a randomized controlled trial (RCT) of 452 patients presenting at a Swiss ED – the B-type Natriuretic Peptide for Acute Shortness of Breath Evaluation (BASEL) study – showed that those assigned to receive rapid, point-of-care BNP testing were discharged faster (8 vs. 11 days, p=0.001) than those assigned to standard assessment [1].
Results also showed that the percentage of patients requiring hospitalization dropped from 85 % to 75 % and those admitted to intensive care dropped from 24 % to 15 % [1]. Although mortality rates were not significantly lower (10 % vs. 12 %, p=0.45), the mean cost of treatment was reduced significantly in the BNP group (USD 5,410 vs. 7,264, p=0.006) [1].
|
In tests to rule out heart failure, NT-proBNP has been demonstrated to be a cost-effective measure with good diagnostic properties. A Canadian RCT – Improved Management of Patients with Congestive Heart Failure (IMPROVE-CHF) study – investigated the clinical diagnosis with or without NT-proBNP testing. With the addition of NT-proBNP testing shorter ED visits, reduced costs of 15 % overall, as well as fewer rehospitalizations (decrease of 35 %) among patients with acute heart failure was seen over 60 days [3]. The N-terminal Pro-BNP investigation of Dyspnea in the Emergency Department (PRIDE) study confirmed NP testing to be particularly useful in cases where there is a high degree of uncertainty about a diagnosis – this group also represent the patients with the poorest prognosis [13,14]. This same study also showed that including NT-proBNP measurement was superior to routine chest radiograph (CXR) interpretation in conjunction with clinical judgment for diagnosis or exclusion of acute heart failure. However, it should be noted that a 2011 meta-analysis of RCTs reported inconsistent results regarding the impact of systematic NP testing on time to discharge and costs, indicating that care should be taken in the design and implementation of NP testing protocols to gain the maximum benefits [15]. |
|
PRACTICAL IMPLEMENTATION OF NATRIURETIC PEPTIDE TESTING IN THE EMERGENCY DEPARTMENT
NPs must be considered as part of a wider diagnostic pathway, as an adjunct to clinical assessment. When establishing testing in the ED setting, it is important to reach a consensus about how best to integrate NPs within the individual hospital, and to understand how to interpret NP findings.
Given the key importance of rapid NP results [12], NP levels are best measured at the point of care, but the central lab should play a key role in developing and overseeing testing protocols. The choice of NP to use can be made to suit local needs, since BNP and NT-proBNP appear to be similar in diagnostic accuracy [16-18] and both are recommend for use by the ESC and ACCF/AHA [8,9].
Interpretation of NP results requires knowledge of potential confounders – factors other than heart failure that could cause increased NP levels [7,19].
Due to this variation of NP levels, particularly relating to age, it is easier to rule out heart failure using NPs than to confirm heart failure. 300 pg/mL was an age-independent cut-off for NT-proBNP for ruling out heart failure in the International Collaborative of NT-proBNP Study (ICON), with a 98 % negative predictive value [7]. However, false negatives can still occur, potentially due to: right heart failure, mild heart failure, chronic, more compensated heart failure, nonsystolic heart failure, and obesity. Due to the fact that NT-proBNP values increase with age, adding age stratification greatly improved positive predictive value in ICON – i.e. confirming the presence of heart failure (Table I) [7].
Table I: Optimal NT-proBNP cut-points for the diagnosis or exclusion of acute heart failure among dyspneic patients
Adapted from Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NTproBNP Study. Eur Heart J 2006; 27: 330-7.
In gray areas, other disease patterns such as pulmonary embolism or pneumonia must also be considered in the differential diagnosis as these conditions can also result in an increase in the marker (Table I) [7]. Recommendations from Januzzi et al. for the overall integration of NP measures into acute dyspnea diagnostic pathways are shown in Figure 2 [6].
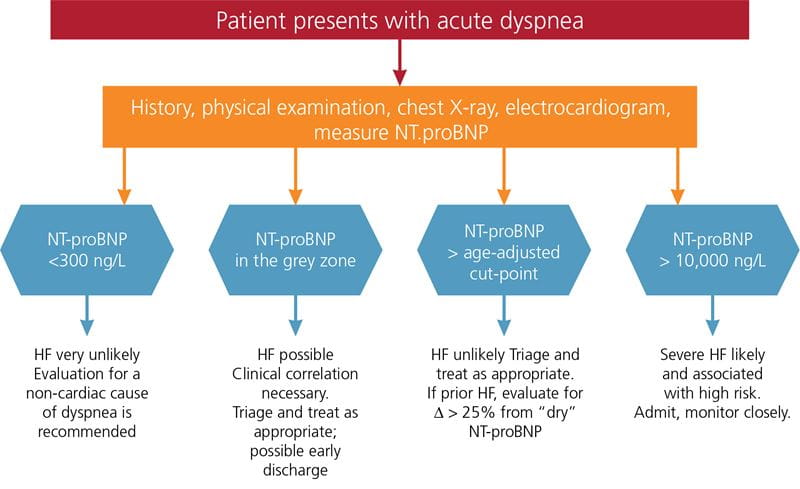
FIG. 2: Recommendations for integrating NP measures into diagnosis for patients presenting with acute dyspnea
Adapted from Januzzi JL, Chen-Tournoux AA, Moe G. Amino-terminal pro-B-type natriuretic peptide testing for the diagnosis or exclusion of heart failure in patients with acute symptoms. Am J Cardiol 2008; 101(Suppl): 29A-38A.
THE ROLE OF NATRIURETIC PEPTIDES WITHIN INPATIENT AND OUTPATIENT CARDIAC CARE
Once a patient has been admitted, NPs can play a role in monitoring treatment success and discharge planning. BNP levels were observed to decrease in correlation with falling pulmonary capillary edge pressure in a study of patients being treated for decompensated heart failure, which suggested a role in monitoring response to therapy [20].
In the Efficacy and Safety of Relaxin for the Treatment of Acute Heart Failure (RELAX-AHF) study, patients who achieved less than a 30 % decrease in NT-proBNP from Day 0 to Day 2 of treatment with serelaxin had an increased 180-day-all-cause-mortality vs. patients who achieved a greater decrease [20]. However, NPs might not be appropriate for monitoring success of all heart failure therapies. A study of nesiritide infusion showed that most patients who did achieve a clinical response did not show a significant decrease in BNP/NTproBNP levels [22].
Several studies have confirmed that NP levels at discharge (more than at admission) are prognostic for mortality and/or readmission, giving helpful guidance on the appropriate time for discharge according to the risk of future complications [23-30].
In the outpatient setting, BNP and NT-proBNP are promising tests to optimize chronic heart failure management, aiming to reduce readmissions and death. Two meta-analyses of RCTs testing therapy guided by NP levels (i.e. up-titrating therapy to achieve a certain level of or reduction in NP levels) have shown that this strategy led to significantly reduced all-cause mortality and heart failure-related hospitalizations vs. clinically guided therapy [31,32].
This strategy is now being tested in a large, US NIH-funded RCT called Guiding Evidence Based Therapy Using Biomarker Intensified Treatment (GUIDE-IT). GUIDE-IT is examining a strategy of titrating medical therapy based on minimizing NP levels in comparison with usual care, in high risk heart failure patients with left ventricular systolic dysfunction [33]. The primary endpoint is a composite of heart failure hospitalizations or cardiovascular mortality [33]. The planned recruitment is 1,100 patients, and the final data collection for the primary endpoint is expected in September 2017 [33].
CONCLUSIONS
NT-proBNP and BNP are biomarkers for heart failure in patients with dyspnea that have the potential to improve diagnostic accuracy in EDs, speed up and enhance management and admission decisions, and ultimately, improve outcomes and reduce costs when successfully integrated into care pathways [1,3,4,6,7]. Diagnostic thresholds have been developed that make this integration straightforward.
NPs should always be used as an adjunct to clinical assessment, rather than a replacement. Central labs and other stakeholders should play a key role in developing and overseeing point-of-care testing protocols [6-8].
NPs can help indicate the optimum time for patient discharge, and act as a prognostic tool to inform the future risk of heart failure events upon patient discharge, as well as the success of some heart failure treatments [8,9,13,14].
The potential for NPs to guide up-titration of heart failure therapy is supported by an increasing body of evidence, and is currently being assessed in GUIDE-IT [33].
References+ View more
- Mueller C, Scholer A, Laule-Kilian K, et al. Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med 2004; 350: 647-54.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA 2013; 309: 355-63.
- Moe GW, Howlett J, Januzzi JL, et al. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation 2007; 115: 3103-10.
- Kim H-N, Januzzi JL. Natriuretic peptide testing in heart failure. Circulation 2011; 123: 2015-9.
- Martinez-Rumayor A, Richards AM, Burnett JC, Januzzi JL. Biology of the natriuretic peptides. Am J Cardiol 2008; 101[Suppl]: 3A-8A).
- Januzzi JL, Chen-Tournoux AA, Moe G. Amino-terminal pro-B-type natriuretic peptide testing for the diagnosis or exclusion of heart failure in patients with acute symptoms. Am J Cardiol 2008; 101(Suppl): 29A-38A.
- Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NTproBNP Study. Eur Heart J 2006; 27: 330-7.
- McMurray JJ V, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart. Eur Heart J 2012; 33: 1787-847.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure. Circulation 2013; 128: 000-000.
- Ray P, Birolleau S, Lefort Y, et al. Acute respiratory failure in the elderly: etiology, emergency diagnosis and prognosis. Crit Care 2006; 10: R82.
- Maisel A, Hollander JE, Guss D, et al. Primary results of the Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT). A multicenter study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breath. J Am Coll Cardiol 2004; 44: 1328-33.
- Maisel AS, Peacock WF, McMullin N, et al. Timing of immunoreactive B-type natriuretic peptide levels and treatment delay in acute decompensated heart failure: an ADHERE (Acute Decompensated Heart Failure National Registry) analysis. J Am Coll Cardiol 2008; 52: 534-40.
- Steinhart B, Thorpe KE, Bayoumi AM, et al. Improving the diagnosis of acute heart failure using a validated prediction model. J Am Coll Cardiol 2009; 54: 1515-21.
- Green SM, Martinez-Rumayor A, Gregory S, et al. Clinical uncertainty, diagnostic accuracy, and outcomes in emergency department patients presenting with dyspnea. ArchIntern Med 2008; 168: 741-8.
- Trinquart L, Ray P, Riou B, et al. Natriuretic peptide testing in EDs for managing acute dyspnea: a meta-analysis. Am J Emerg Med 2011; 29: 757-67.
- Mueller T, Gegenhuber A, Poelz W, et al. Diagnostic accuracy of B type natriuretic peptide and amino terminal proBNP in the emergency diagnosis of heart failure. Heart 2005; 91: 606-12.
- Chenevier-Gobeaux C, Claessens Y-E, Voyer S, et al. Influence of renal function on N-terminal pro-brain natriuretic peptide (NT-proBNP) in patients admitted for dyspnoea in the Emergency Department: comparison with brain natriuretic peptide (BNP). Clin Chimica Acta 2005; 361: 167-75.
- Alibay Y, Beauchet A, El Mahmoud R, et al. Plasma N-terminal pro-brain natriuretic peptide and brain natriuretic peptide in assessment of acute dyspnea. Biomed Pharmacother 2005; 59: 20-4.
- Baggish AL, van Kimmenade RR, Januzzi JL. The differential diagnosis of an elevated amino-terminal pro-B-type natriuretic peptide level. Am J Cardiol 2008; 101[Suppl]: 43A-48A.
- Kazanegra R, Cheng V, Garcia A, et al. A rapid test for B-type natriuretic peptide correlates with falling wedge pressures in patients treated for decompensated heart failure: a pilot study. J Card Fail 2001; 7: 21-9.
- Metra M, Cotter G, Davison BA, et al. Effect of serelaxin on cardiac, renal, and hepatic biomarkers in the Relaxin in Acute Heart Failure (RELAX-AHF) development program: correlation with outcomes. J Am Coll Cardiol 2013; 61: 196-206.
- Miller WL, Hartman KA, Burritt MF, et al. Biomarker responses during and after treatment with nesiritide infusion in patients with decompensated chronic heart failure. Clin Chem 2005; 51: 569-77.
- Logeart D, Thabut G, Jourdain P, et al. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol 2004; 43: 635-41.
- Waldo SW, Beede J, Isakson S, et al. Pro-B-type natriuretic peptide levels in acute decompensated heart failure. J Am Coll Cardiol 2008; 51: 1874-82.
- Cohen-Solal A, Logeart D, Huang B, et al. Lowered B-type natriuretic peptide in response to levosimendan or dobutamine treatment is associated with improved survival in patients with severe acutely decompensated heart failure. J Am Coll Cardiol 2009; 53: 2343-8.
- O’Connor CM, Hasselblad V, Mehta RH, et al. Triage after hospitalization with advanced heart failure: the ESCAPE (Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness) risk model and discharge score. J Am Coll Cardiol 2010; 55: 872-8.
- Kociol RD, Horton JR, Fonarow GC, et al. Admission, discharge, or change in B-type natriuretic peptide and long-term outcomes: data from Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) linked to Medicare claims. Circ Heart Fail 2011; 4: 628-36.
- Bettencourt P, Azevedo A, Pimenta J, Friões F, Ferreira S, Ferreira A. N-terminal-pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation 2004; 110: 2168-74.
- Verdiani V, Nozzoli C, Bacci F, Cecchin A, Rutili MS, Paladini S, Olivotto I. Pre-discharge B-type natriuretic peptide predicts early recurrence of decompensated heart failure in patients admitted to a general medical unit. Eur J Heart Fail 2005; 7: 566-71.
- Noveanu M, Breidthardt T, Potocki M, et al. Direct comparison of serial B-type natriuretic peptide and NT-proBNP levels for prediction of short- and long-term outcome in acute decompensated heart failure. Crit Care 2011; 15: R1.
- Savarese G, Trimarco B, Dellegrottaglie S, et al. Natriuretic peptide-guided therapy in chronic heart failure: a metaanalysis of 2,686 patients in 12 randomized trials. PloS One 2013;8:e58287.
- Felker GM, Hasselblad V, Hernandez AF, et al. Biomarker-guided therapy in chronic heart failure: a meta-analysis of randomized controlled trials. Am Heart J 2009; 158: 422-30.
- National Institutes of Health. Guiding Evidence Based Therapy Using Biomarker Intensified Treatment (GUIDE-IT). NCT 1685840. http://clinicaltrials.gov/ct2/show/NCT01685840. Accessed 03.09.2013.
References
- Mueller C, Scholer A, Laule-Kilian K, et al. Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med 2004; 350: 647-54.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA 2013; 309: 355-63.
- Moe GW, Howlett J, Januzzi JL, et al. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation 2007; 115: 3103-10.
- Kim H-N, Januzzi JL. Natriuretic peptide testing in heart failure. Circulation 2011; 123: 2015-9.
- Martinez-Rumayor A, Richards AM, Burnett JC, Januzzi JL. Biology of the natriuretic peptides. Am J Cardiol 2008; 101[Suppl]: 3A-8A).
- Januzzi JL, Chen-Tournoux AA, Moe G. Amino-terminal pro-B-type natriuretic peptide testing for the diagnosis or exclusion of heart failure in patients with acute symptoms. Am J Cardiol 2008; 101(Suppl): 29A-38A.
- Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NTproBNP Study. Eur Heart J 2006; 27: 330-7.
- McMurray JJ V, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart. Eur Heart J 2012; 33: 1787-847.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure. Circulation 2013; 128: 000-000.
- Ray P, Birolleau S, Lefort Y, et al. Acute respiratory failure in the elderly: etiology, emergency diagnosis and prognosis. Crit Care 2006; 10: R82.
- Maisel A, Hollander JE, Guss D, et al. Primary results of the Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT). A multicenter study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breath. J Am Coll Cardiol 2004; 44: 1328-33.
- Maisel AS, Peacock WF, McMullin N, et al. Timing of immunoreactive B-type natriuretic peptide levels and treatment delay in acute decompensated heart failure: an ADHERE (Acute Decompensated Heart Failure National Registry) analysis. J Am Coll Cardiol 2008; 52: 534-40.
- Steinhart B, Thorpe KE, Bayoumi AM, et al. Improving the diagnosis of acute heart failure using a validated prediction model. J Am Coll Cardiol 2009; 54: 1515-21.
- Green SM, Martinez-Rumayor A, Gregory S, et al. Clinical uncertainty, diagnostic accuracy, and outcomes in emergency department patients presenting with dyspnea. ArchIntern Med 2008; 168: 741-8.
- Trinquart L, Ray P, Riou B, et al. Natriuretic peptide testing in EDs for managing acute dyspnea: a meta-analysis. Am J Emerg Med 2011; 29: 757-67.
- Mueller T, Gegenhuber A, Poelz W, et al. Diagnostic accuracy of B type natriuretic peptide and amino terminal proBNP in the emergency diagnosis of heart failure. Heart 2005; 91: 606-12.
- Chenevier-Gobeaux C, Claessens Y-E, Voyer S, et al. Influence of renal function on N-terminal pro-brain natriuretic peptide (NT-proBNP) in patients admitted for dyspnoea in the Emergency Department: comparison with brain natriuretic peptide (BNP). Clin Chimica Acta 2005; 361: 167-75.
- Alibay Y, Beauchet A, El Mahmoud R, et al. Plasma N-terminal pro-brain natriuretic peptide and brain natriuretic peptide in assessment of acute dyspnea. Biomed Pharmacother 2005; 59: 20-4.
- Baggish AL, van Kimmenade RR, Januzzi JL. The differential diagnosis of an elevated amino-terminal pro-B-type natriuretic peptide level. Am J Cardiol 2008; 101[Suppl]: 43A-48A.
- Kazanegra R, Cheng V, Garcia A, et al. A rapid test for B-type natriuretic peptide correlates with falling wedge pressures in patients treated for decompensated heart failure: a pilot study. J Card Fail 2001; 7: 21-9.
- Metra M, Cotter G, Davison BA, et al. Effect of serelaxin on cardiac, renal, and hepatic biomarkers in the Relaxin in Acute Heart Failure (RELAX-AHF) development program: correlation with outcomes. J Am Coll Cardiol 2013; 61: 196-206.
- Miller WL, Hartman KA, Burritt MF, et al. Biomarker responses during and after treatment with nesiritide infusion in patients with decompensated chronic heart failure. Clin Chem 2005; 51: 569-77.
- Logeart D, Thabut G, Jourdain P, et al. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol 2004; 43: 635-41.
- Waldo SW, Beede J, Isakson S, et al. Pro-B-type natriuretic peptide levels in acute decompensated heart failure. J Am Coll Cardiol 2008; 51: 1874-82.
- Cohen-Solal A, Logeart D, Huang B, et al. Lowered B-type natriuretic peptide in response to levosimendan or dobutamine treatment is associated with improved survival in patients with severe acutely decompensated heart failure. J Am Coll Cardiol 2009; 53: 2343-8.
- O’Connor CM, Hasselblad V, Mehta RH, et al. Triage after hospitalization with advanced heart failure: the ESCAPE (Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness) risk model and discharge score. J Am Coll Cardiol 2010; 55: 872-8.
- Kociol RD, Horton JR, Fonarow GC, et al. Admission, discharge, or change in B-type natriuretic peptide and long-term outcomes: data from Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) linked to Medicare claims. Circ Heart Fail 2011; 4: 628-36.
- Bettencourt P, Azevedo A, Pimenta J, Friões F, Ferreira S, Ferreira A. N-terminal-pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation 2004; 110: 2168-74.
- Verdiani V, Nozzoli C, Bacci F, Cecchin A, Rutili MS, Paladini S, Olivotto I. Pre-discharge B-type natriuretic peptide predicts early recurrence of decompensated heart failure in patients admitted to a general medical unit. Eur J Heart Fail 2005; 7: 566-71.
- Noveanu M, Breidthardt T, Potocki M, et al. Direct comparison of serial B-type natriuretic peptide and NT-proBNP levels for prediction of short- and long-term outcome in acute decompensated heart failure. Crit Care 2011; 15: R1.
- Savarese G, Trimarco B, Dellegrottaglie S, et al. Natriuretic peptide-guided therapy in chronic heart failure: a metaanalysis of 2,686 patients in 12 randomized trials. PloS One 2013;8:e58287.
- Felker GM, Hasselblad V, Hernandez AF, et al. Biomarker-guided therapy in chronic heart failure: a meta-analysis of randomized controlled trials. Am Heart J 2009; 158: 422-30.
- National Institutes of Health. Guiding Evidence Based Therapy Using Biomarker Intensified Treatment (GUIDE-IT). NCT 1685840. http://clinicaltrials.gov/ct2/show/NCT01685840. Accessed 03.09.2013.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info.
Acute care testing handbook
Get the acute care testing handbook
Your practical guide to critical parameters in acute care testing.
Download nowRelated webinar
Clinical use of natriuretic peptide
Presented by Dr James Januzzi, Mass General, USA Watch the webinarRelated webinar
Natriuretic Peptides: A Cardiologist's View
Presented by Dr. Christopher deFilippi, Cardiologist, University of Maryland School of Medicine, Baltimore, MD Watch the webinarRelated webinar
Usefulness of B-Type Natriuretic Peptides in Emergency Medicine
An Emergency Department Point of View. Presented by Dr. Patrick Ray, Emergency Physician, Hospital Tenon, Paris, France Watch the webinarScientific webinars
Check out the list of webinars
Radiometer and acutecaretesting.org present free educational webinars on topics surrounding acute care testing presented by international experts.
Go to webinars