Printed from acutecaretesting.org
December 2014
Role of POCT in the management of patients with acute dyspnea
Acute dyspnea is the key symptom of about 5-10 % of patients presenting to the emergency department (ED) [1-7]. In contrast to common thinking, the mortality of patients presenting with acute dyspnea is even higher than that of patients presenting with acute chest pain.
In addition, dyspnea is a challenging symptom with more than 30 possible underlying diagnoses. Acute heart failure (AHF) is responsible for about 50 % of all cases and therefore requires particular attention (Fig. 1).
Pneumonia, exacerbated COPD and asthma, pulmonary embolism and anemia are also common [1-5]. Early and accurate diagnosis of AHF is particularly challenging in patients with a history of both cardiac and obstructive pulmonary disease.
Delays in establishing the correct diagnosis and appropriate treatment may influence subsequent length of hospital stay, morbidity and mortality [1-7].
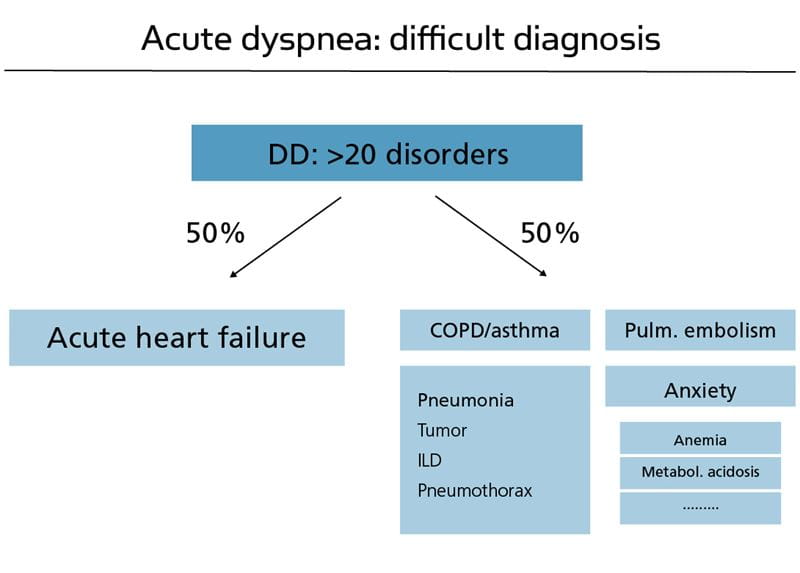
Fig. 1: Acute heart failure is the most common disease underlying acute dyspnea
The diagnostic process includes three steps. First, ensuring that AHF is the cause of acute dyspnea. This first step relies on clinical judgment to integrate patient history, physical examination, investigations including chest x-ray, the 12-lead ECG, as well as elevated levels of natriuretic peptides [1-5].
In the ED, as well as in the primary care setting, measurement of natriuretic peptides has been demonstrated to be extremely helpful in the diagnosis/exclusion of AHF and to support treatment and referral decisions (Fig. 2).
Cardiac imaging with echocardiography is key in the second step in order to define the underlying cardiac pathology. If natriuretic peptides are available and in the absence of shock, echocardiography can usually be deferred to the second day (Fig. 3).
Step three in the diagnostic process starts in the ED and aims to establish the trigger of AHF, as this will offer additional treatment options, e.g. antibiotics for sepsis.
For an efficient diagnostic process, it is also critical that there is consensus among the different healthcare providers regarding the diagnostic tests and criteria adopted in their specific facility.
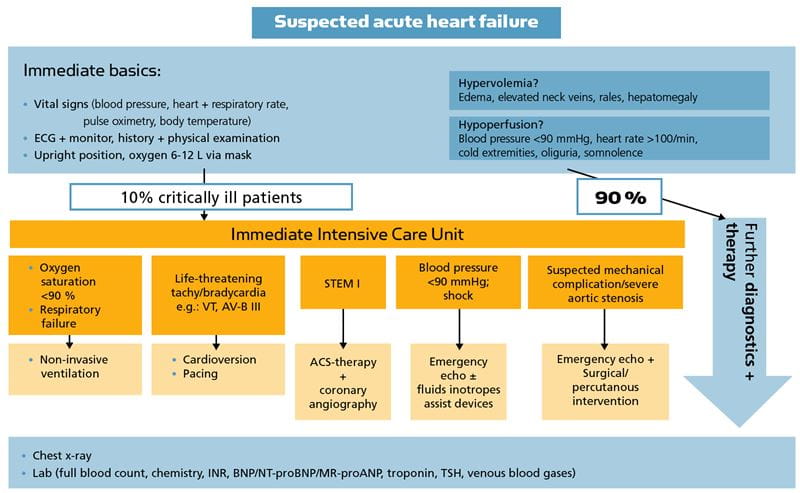
Fig. 2: Biomarkers complement clinical assessment and other diagnostic tools in the assessment of patients with suspected acute heart failure.
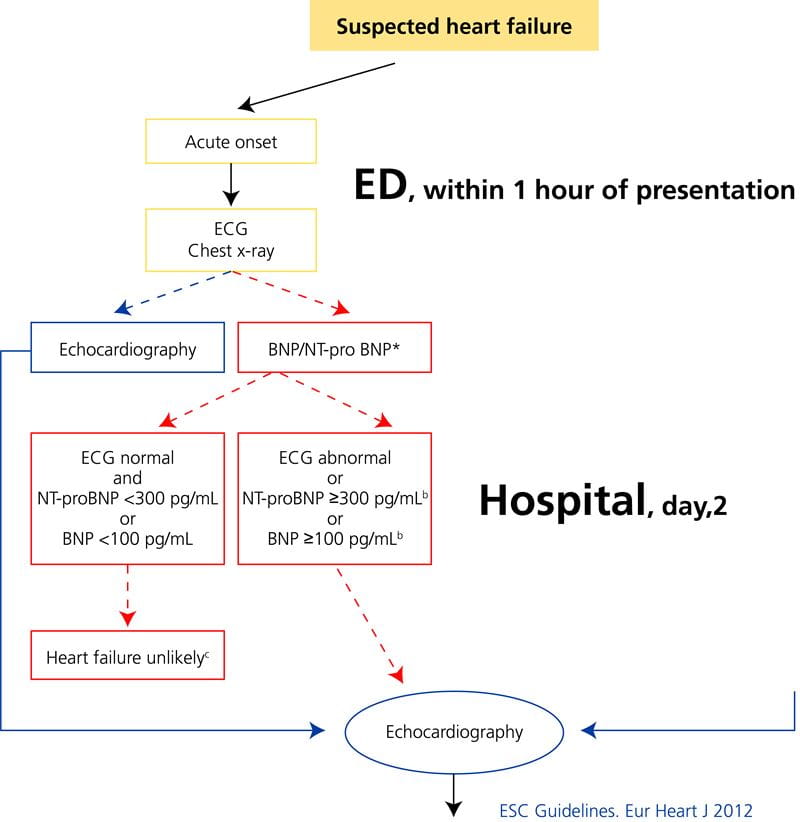
Fig. 3: Current ESC guidelines highlight the importance of the early measurement of natriuretic peptides in patients with dyspnea.
In recent years several studies have shown the added value of natriuretic peptides, quantitative markers of hemodynamic cardiac stress and HF in the early diagnosis of AHF.
Three NPs have become clinically available: B-type NP (BNP), N-terminal pro-B-type NP (NT-proBNP), and midregional pro-atrial NP (MR-proANP). All three have been shown to have high and comparable diagnostic accuracy for AHF.
NPs are released from the left and right ventricle as well as from the atria in response to pressure or volume overload.
Hence levels increase according to the severity of HF, their levels seem to integrate the presence and extent of left-ventricular systolic dysfunction, left-ventricular diastolic dysfunction, valvular dysfunction and right-ventricle dysfunction.
The medical as well as economic benefits of using NPs in patients with suspected AHF have been documented in several randomized controlled studies. These data justify the liberal use of NPs in all patients presenting with acute dyspnea.
Levels should be obtained with the initial routine blood draw in order to allow them to be available to clinicians as soon as possible. This is now also reflected in current guidelines.
Natriuretic peptide levels should be interpreted as a quantitative variable with higher levels indicating a higher likelihood for AHF being the main cause of acute dyspnea.
Obesity has been recently identified to be an important confounder in the interpretation of BNP and NT-proBNP levels [8]. Levels in obese patients are much lower than in normal-weight patients. Therefore, they need to be multiplied by about 2 in order to obtain levels that fit into the recommended interpretation algorithm [7].
Pulmonary embolism is the underlying cause of acute dyspnea in 5-10 % of patients.
As symptoms are very unspecific, a diagnostic strategy combining the assessment of pretest probability, D-dimers and CT angiography is applied in all patients with suspected pulmonary embolism.
In contrast to natriuretic peptides, D-dimers should not be measured in all patients with acute dyspnea, but only in those with suspected pulmonary embolism.
Anemia is a common confounder of cardiac and pulmonary disease in patients with acute dyspnea, but very rarely the sole cause in patients with dyspnea as their main symptom.
Venous (not arterial) blood gases provide insights regarding the presence of metabolic acidosis, as well as CO2 retention. With the wide availability of pulse oximetry, arterial puncture and measurement of pO2(a) can be restricted to patients in whom no reliable pulse oximetry signal can be obtained and to patients with some intoxications.
In conclusion, state-of-the-art POCT technology helps physicians to rapidly identify the cause of acute dyspnea. Natriuretic peptides and hemoglobin should be obtained in all, D-dimers and venous blood gases in most patients.
References+ View more
- Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002; 347(3): 161-7.
- Januzzi Jr JL, , Sakhuja R, O'Donoghue M, Baggish AL, Anwaruddin S, Chae CU, et al. Utility of amino-terminal pro-brain natriuretic peptide testing for prediction of 1-year mortality in patients with dyspnea treated in the emergency department. Arch Intern Med 2006; 166(3): 315-20.
- Maisel A, Mueller C, Nowak RM, Peacock WF, Ponikowski P, Mockel M, et al. Midregion prohormone adrenomedullin and prognosis in patients presenting with acute dyspnea: results from the BACH (Biomarkers in Acute Heart Failure) trial. J Am Coll Cardiol 2011; 58(10): 1057-67.
- Mueller C, Laule-Kilian K, Scholer A, Frana B, Rodriguez D, Schindler C, et al. Use of B-type natriuretic peptide for the management of women with dyspnea. J Am Coll Card 2004; 94(12): 1510-4.
- Moe GW, Howlett J, Januzzi JL, Zowall H, Canadian Multicenter Improved Management of Patients With Congestive Heart Failure Study I. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation 2007; 115(24): 3103-10.
- Rutten JH, Steyerberg EW, Boomsma F, van Saase JL, Deckers JW, Hoogsteden HC, et al. N-terminal pro-brain natriuretic peptide testing in the emergency department: beneficial effects on hospitalization, costs, and outcome. Am Heart J 2008; 156(1): 71-77
- Writing Committee M, Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr., et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128(16): e240-327.
- Daniels LB, Clopton P, Bhalla V, Krishnaswamy P, Nowak RM, McCord J, et al. How obesity affects the cut-points for B-type natriuretic peptide in the diagnosis of acute heart failure. Results from the Breathing Not Properly Multinational Study. Am Heart J 2006; 151(5): 999-1005.
References
- Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002; 347(3): 161-7.
- Januzzi Jr JL, , Sakhuja R, O'Donoghue M, Baggish AL, Anwaruddin S, Chae CU, et al. Utility of amino-terminal pro-brain natriuretic peptide testing for prediction of 1-year mortality in patients with dyspnea treated in the emergency department. Arch Intern Med 2006; 166(3): 315-20.
- Maisel A, Mueller C, Nowak RM, Peacock WF, Ponikowski P, Mockel M, et al. Midregion prohormone adrenomedullin and prognosis in patients presenting with acute dyspnea: results from the BACH (Biomarkers in Acute Heart Failure) trial. J Am Coll Cardiol 2011; 58(10): 1057-67.
- Mueller C, Laule-Kilian K, Scholer A, Frana B, Rodriguez D, Schindler C, et al. Use of B-type natriuretic peptide for the management of women with dyspnea. J Am Coll Card 2004; 94(12): 1510-4.
- Moe GW, Howlett J, Januzzi JL, Zowall H, Canadian Multicenter Improved Management of Patients With Congestive Heart Failure Study I. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation 2007; 115(24): 3103-10.
- Rutten JH, Steyerberg EW, Boomsma F, van Saase JL, Deckers JW, Hoogsteden HC, et al. N-terminal pro-brain natriuretic peptide testing in the emergency department: beneficial effects on hospitalization, costs, and outcome. Am Heart J 2008; 156(1): 71-77
- Writing Committee M, Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr., et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128(16): e240-327.
- Daniels LB, Clopton P, Bhalla V, Krishnaswamy P, Nowak RM, McCord J, et al. How obesity affects the cut-points for B-type natriuretic peptide in the diagnosis of acute heart failure. Results from the Breathing Not Properly Multinational Study. Am Heart J 2006; 151(5): 999-1005.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info.
Acute care testing handbook
Get the acute care testing handbook
Your practical guide to critical parameters in acute care testing.
Download nowRelated webinar
Evolution of blood gas testing Part 1
Presented by Ellis Jacobs, PhD, Assoc. Professor of Pathology, NYU School of Medicine.
Watch the webinar









