Printed from acutecaretesting.org
October 2010
"Permissive hypercapnia" finding its place in clinical care
HAS THIS EVER HAPPENED TO YOU?
You are working in a busy emergency room or ICU, and you've just run the blood gas of Mrs Jones. The pH comes back as 7.21, and the pCO2 comes back as 60 mmHg. In your institution these are critical lab values that must be reported to the responsible clinician.
You stat page the prescribing physician and read the results. As you await orders to address this, she tells you, "Thank you; we are fine with these values." You are surprised at this response; and you might think, "What gives?"
What "gives" is this: without knowing the full clinical picture for Mrs Jones, a single set of lab measurements – in this case, the acidic pH of 7.21 and/or pCO2 of 60 mmHg – may or may not be particularly actionable. This is the underlying thinking behind "permissive hypercapnia", explained by this definition:
"An approach to the management of acute respiratory failure in which the tidal volume (VT ) is lower – 5-8 mL/kg than that conventionally used – 10-15 mL/kg; the arterial pCO2 is allowed to rise above the "normal" of 40 mmHg, and no attempts are made to compensate for subsequent changes in blood pH–respiratory acidosis." [1]
The focus of this article is a discussion of permissive hypercapnia (also known as therapeutic hypercapnia or permissive hypercapnic acidosis) within the context of mechanical ventilation.
Going back to our scenario, it is not that a pH of 7.21 would be unimportant; it still must be monitored. But according to Madhu Sasidhar, MD, section head for Respiratory Care at the Cleveland Clinic in Ohio (USA), the importance of the pH or pCO2 depends on the underlying disease state.
"In the context of mechanical ventilation, it is widely accepted that you can have a low pH," he says. "However, this is disease-specific; for example we might accept this value with obstructive lung disease or ARDS [acute respiratory distress syndrome] but not in patients with certain neurological diseases."
Dr Sasidhar adds that when determining how far a clinician will go in sustaining permissive hypercapnia, the possibility for significant lung injury is often weighed against the harm that may or may not occur when attempting to maintain a "normal" carbon dioxide (CO2) level.
"In maintaining ventilation parameters to a normal CO2," he says, "we want to avoid [causing or] worsening lung injury. From a practical standpoint, the question is, 'What is worse: hypercapnia or excessive tidal volume?'"
A number of studies have attempted to answer that question. In 1999, Laffey et al [2] asked, "Carbon dioxide and the critically ill – too little of a good thing?" They looked at the possibility that increased pCO2(a) "may be a goal of therapy in critical illness, rather than something to be avoided."
They reiterated the fact that "death in ARDS results largely from multisystem organ failure, not hypoxia," which is of course well known.
Interestingly they also explained that "long-term neurological sequelae from exposure in extreme [altitudes]" are the result of "extremely" low pCO2(a) levels, not low oxygen levels. [2]
The accompanying figure illustrates a number of potential mechanisms by which hypercapnia may be protective in organ injury.
FIGURE: Acidosis attenuates a number of inflammatory processes (left) may reduce oxygen consumption (center) and have other positive overall effects (right).
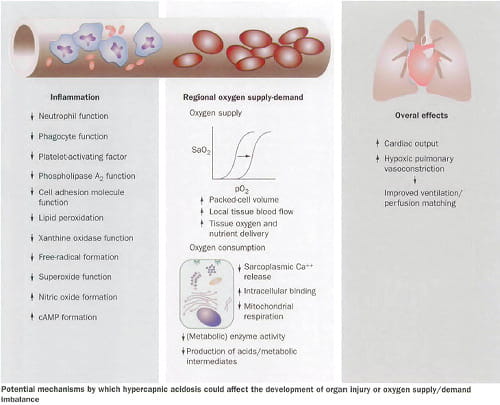
Reprinted from The Lancet; Laffey et al. [2]; Copyright (2010), with permission from Elsevier
Laffey and colleagues suggested what was then a new idea: "…a potentially novel strategy – therapeutic hypercapnia – whereby hypercapnia could be intentionally produced in critically ill patients to provide organ protection." [2]
In a more recent editorial discussing therapeutic hypercapnia and sepsis, [3] Swenson, while acknowledging that permissive hypercapnia can have a positive effect in some cases, posed a caution:
There is a concern that "therapeutic hypercapnia may impair host defenses against pathogens surely to be encountered by mechanically ventilated patients." [3]
IF YOU CAN MEASURE IT…?
Swenson [3] also gives some important historical context to the issue of permissive hypercapnia, pointing out that when blood gas analysis became available almost 60 years ago, it "revealed surprisingly profound hypercapnia." An example he notes: "a (pCO2(a) > 150 mmHg) [with a pH of 7] without negative consequences involving one-lung ventilation."
And yet, with this ability to measure blood gas parameters it was almost 30 years before permissive hypercapnia was studied, he adds.
And while there appear to be many positives, "[some] have reported … proinflammatory effects … making the case less than solid in favor of therapeutic hypercapnia." [3]
This has led some researchers to wonder whether hypercapnia, even though it is a part of "ventilatory strategies that reduce lung stretch resulting in [permissive hypercapnia and improving] outcome[s]" is "a double-edged sword." [4]
So it makes sense to proceed with caution when measuring and managing carbon dioxide levels and in tolerating levels of hypercapnia. That said, it has therapeutic value. As Curley and colleagues note, [5] "hypocapnia remains a common – and generally underappreciated – component of many disease states."
They add that "hypocapnia may be a pathogenic entity in the setting of critical illness." [5]
REASONABLE CLINICAL GOALS?
With the issues surrounding the use of this technique, the question naturally arises, "What are reasonable clinical goals for hypercapnia?" According to Dr Sasidhar, "Reasonable clinical goals would indicate a pCO2 as a function of the bicarbonate level."
For example, he says, "There is literature that indicates that you can go lower than a pH of 7.2. I would caution that you would want to see adequate renal function. For example, a bicarbonate level in the low 40s may allow you to tolerate a pCO2 of 70 to 80 mmHg resulting in an acceptable pH."
In the absence of adequate renal compensation, he adds, the clinician should consider giving the patient supplemental bicarbonate.
Higgins et al [6] also weigh in on buffering and renal function, "when hypercapnia persists … renal compensation of the hypercapnic acidosis gradually corrects the pH close to the normal range." In this particular study, they looked at the effect of "the contribution of the acidosis versus hypercapnia per se…"
They sought to determine whether "the acidosis produced by acute hypercapnia should be buffered." [6] They found that hypercapnic acidosis reduced the severity of sepsis-induced lung injury.
Also, both buffered hypercapnia and hypercapnic acidosis weakened the hemodynamic sequelae of systemic sepsis. [6]
WHAT DOES THE TECHNICIAN NEED TO KNOW?
According to Dr Sasidhar, there are a few important things to know. First he says, understand how your particular blood gas machine works. "Bear in mind that the bicarbonate level, for example, is an indirect measure; the machine does not directly measure this lab value," he advises.
Also, know the accepted pH levels in your institution, and realize that there may be variation, both by clinician and by disease state. "Know what those pH levels are, and understand that the clinician may approve a certain pH, particularly let's say, if the target for CO2 may be 70 to 80," he advises.
"It is not always in the patient's best interest to push the pH upwards." That said, however, Dr Sasidhar cautions that some conditions contraindicate permissive hypercapnic conditions.
"In certain neurological conditions, for example, hypercapnia is not appropriate," Dr Sasidhar says. And Swenson [3] cautions, "the ability to withstand hypercapnic acidosis depends on a strong neuroendocrine response that maintains [cardiac output and blood pressure despite the effects of excess] carbon dioxide."
Also keep in mind that a patient on continuous renal replacement therapy (CRRT) will have a low pH for the first 3 days," says Dr Sasidhar, "as it usually takes those first 3 days to achieve the target bicarbonate level."
This is where knowledge of the entire clinical picture is, again, imperative.
This latter observation prompted Dr Sasidhar and colleagues to embark on a study that will look at the role of dialysis in the management and adjustment of pH, with all the attendant clinical effects.
When it comes to hypercapnia, "there are a number of clinicians trying to adjust the pH," he says. "The nephrologists and renal technicians are attempting to adjust it via kidney function and the pulmonologists and respiratory therapists are working with respiratory/lung function."
A cautionary note reminds all of us that we need to remember that a number is just a number. In doing what is best for the patient, consider the entire clinical picture, in order to letting "permissive" hypercapnia become "lax" or "out of control."
References+ View more
- The Free Dictionary. Permissive hypercapnia. Retrieved from http://medical-dictionary.thefreedictionary.com/permissive+hypercapnia.
References
- The Free Dictionary. Permissive hypercapnia. Retrieved from http://medical-dictionary.thefreedictionary.com/permissive+hypercapnia.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info.
Acute care testing handbook
Get the acute care testing handbook
Your practical guide to critical parameters in acute care testing.
Download nowRelated webinar
Evolution of blood gas testing Part 1
Presented by Ellis Jacobs, PhD, Assoc. Professor of Pathology, NYU School of Medicine.
Watch the webinar









