Printed from acutecaretesting.org
January 2014
Point-of-care blood gas testing decreases ventilator time of the post isolated coronary artery bypass patient
The purpose of this study was to determine if implementation of rapid point-of-care (POC) arterial blood gas (ABG) testing would decrease mechanical ventilation time for post ISO-CAB surgery patients.
The study design was pre/post comparison and the statistical plans used were descriptive and t-test.
Patient ventilator time and blood gas turnaround time were measured pre and post implementation of POC blood gas testing. Ventilation time was measured as the total time each patient was mechanically ventilated from intubation to the time of successful extubation.
Blood gas turnaround time was measured as the total time from when each arterial blood gas (ABG) sample was collected to the time the results were available to the patient’s care provider.
ISO-CAB surgery was being performed at a large acute care facility. Post ISO-CAB patients were admitted post surgery to the ICU/CCU mechanically ventilated. All ABG samples from these patients were sent STAT to the main clinical lab for analysis.
From June 2011 to October 2011, 58 ISO-CAB patients were admitted to the ICU/CCU. The average turnaround time for ABG tests on these patients was 27 minutes and the average time these patients spent on a ventilator was 12 hours.
A POC blood gas testing process was implemented in the ICU/CCU in November 2011. Two hand-held POC analyzers were installed in the unit. Respiratory therapists were trained by laboratory staff to perform blood gas analysis at the patients’ bedside. Laboratory staff also provided extensive technical oversight of the point-of-care testing process.
From December 2011 to September 2012, 122 ISO-CAB patients were admitted to the ICU/CCU. ABG samples were tested using the POC process at the patients’ bedside. The average turnaround time for STAT ABG analysis was 2 minutes. The average time each patient spent mechanically ventilated in the unit was 9 hours.
Implementation of a hand-held, bedside POC arterial blood gas testing process significantly decreased blood gas test turnaround time from 27 minutes to 2 minutes (p < 0.001) (Fig. 1).
Changing blood gas testing from the traditional laboratory testing process of sending blood gas samples to the main clinical lab for analysis to a bedside POC process is clinically significant. The patient hours spent mechanically ventilated decreased, on average, from 12 hours to 9 hours (Fig. 2).
A decrease in patient ventilator time decreases the patient’s risk of developing ventilator-acquired pneumonia and other adverse complications.
No other process changes were implemented from November 2011 to September 2012. It is hypothesized that the average reduction in turnaround time by 25 minutes for the ABG tests, allowed the respiratory therapists to treat the patients faster, make ventilator changes in a timely manner, and, as a result, wean patients, on average, 3 hours sooner.
Changing blood gas testing from the traditional laboratory testing process of sending blood gas samples to the main clinical lab for analysis to a bedside POC process was also shown to be cost effective. The study showed that ventilation time decreased an average of 3 hours per patient, saving 366 hours of ventilation time (Fig. 2). Based on care provider costs, the estimated cost of a post ISO-CAB patient cost/hour of ICU care was estimated conservatively at $135.
Therefore, eliminating 366 hours of ventilation care saved an estimated $49,410 in hospital costs.
Implementation of POC testing in the critical care unit decreases test turnaround time and increases the speed at which clinical providers can deliver care. This can reduce hospital costs and provide clinically significant patient care improvements.
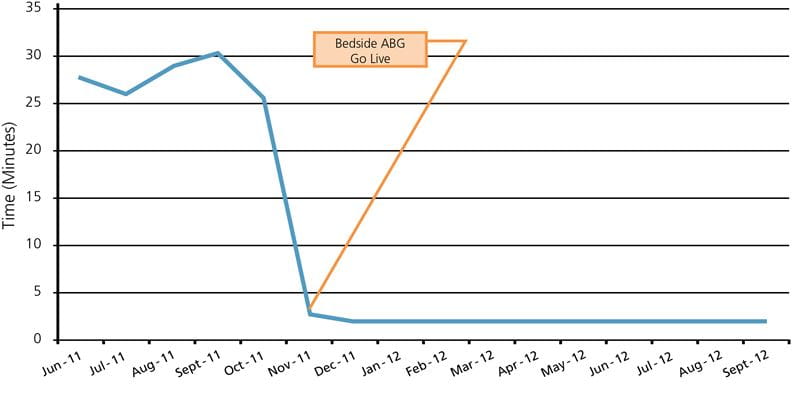
FIG. 1: Blood Gas Turn Around Time Pre and Post Implementation Rapid Bedside Testing
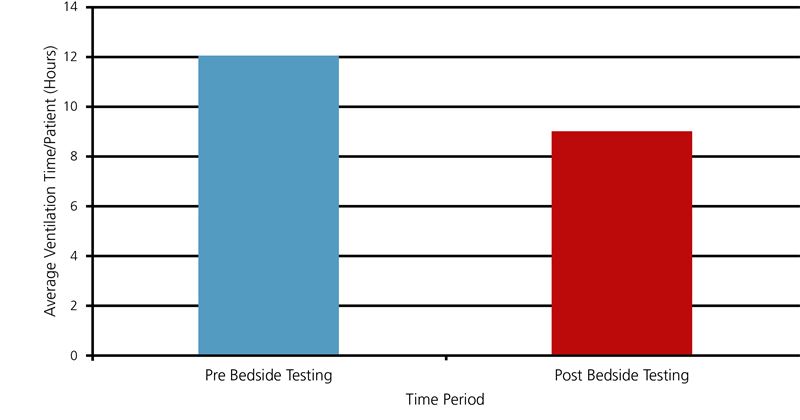
FIG. 2: Ventilation Time Pre and Post Implementation Rapid Bedside Testing
References+ View more
Cheng DC, et al. Morbidity outcome in early versus conventional tracheal extubation after coronary artery bypass grafting: a prospective randomized controlled trial. Journal of Thoracic Cardiovascular Surgeons 1996; 112,3: 755-64. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8800165
Silbert BS, et al. Early extubation following coronary artery bypass surgery. Chest 1998; 113,6: 1481-88. doi:10.1378/chest.113.6.1481
MacIntyre NR, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest 2001: 120, Suppl 6: 375S-395S. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11742959
References
Cheng DC, et al. Morbidity outcome in early versus conventional tracheal extubation after coronary artery bypass grafting: a prospective randomized controlled trial. Journal of Thoracic Cardiovascular Surgeons 1996; 112,3: 755-64. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8800165
Silbert BS, et al. Early extubation following coronary artery bypass surgery. Chest 1998; 113,6: 1481-88. doi:10.1378/chest.113.6.1481
MacIntyre NR, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest 2001: 120, Suppl 6: 375S-395S. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11742959
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info.
Acute care testing handbook
Get the acute care testing handbook
Your practical guide to critical parameters in acute care testing.
Download nowRelated webinar
Evolution of blood gas testing Part 1
Presented by Ellis Jacobs, PhD, Assoc. Professor of Pathology, NYU School of Medicine.
Watch the webinar









